Optic Neuropathy: What Is It & Can You Reverse It?
Home / Neurological Disorders /
Last Updated:
Optic neuropathy is damage to the optic nerve, involving changes to blood flow, harm to structures in the eye, and other underlying causes.
Table of Contents
Symptoms are mostly vision loss, which can be total and sudden. It may involve clouding or blurriness, loss of color vision, loss of peripheral vision, and vision fading in and out.
Damage to the optic nerve can come from disease, malnutrition, chronic inflammation, chronic illnesses, tumors, aneurysms or strokes, injury, genetics, and toxins in the environment. Diagnosing these underlying conditions and treating them will slow down damage to the optic nerve.
Report any symptoms of optic neuropathy to your ophthalmologist or general practitioner. You may not recover the vision you lost, but you can keep the vision you still have.
What Is Optic Neuropathy?
Optic neuropathy is a condition caused by the damage or degradation of the optic nerve. It can lead to blindness.
This eye problem has several underlying causes. These should be treated in order to slow or stop the progression of optic nerve damage.
The problem does not involve inflammation of tissues. Instead, it typically has a range of causes, such as problems with blood supply, like a tumor or aneurysm, a nutritional deficiency, high blood or fluid pressure, or toxic effects from a chemical. It typically only affects one eye.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
What Symptoms Indicate Optic Neuropathy?
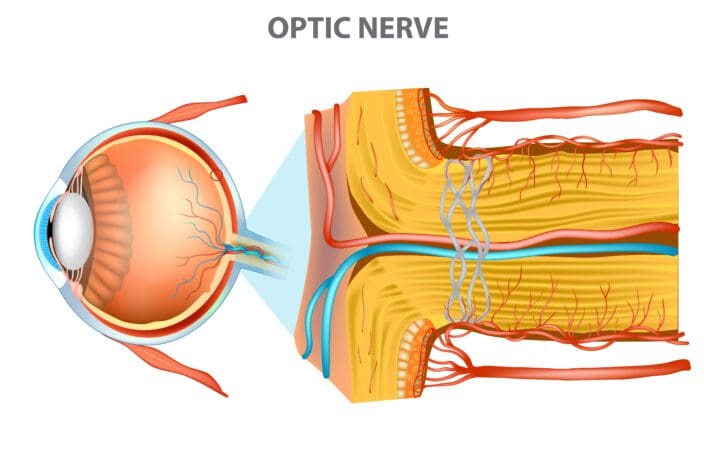
The optic nerve is a bundle of fibers that transmit visual information to the brain after light has been collected in the back of the eye and interpreted first by rods and cones that make up the retina. The main symptom of optic neuropathy is vision loss, which may be so slow in progressing that it is not noticeable until it is significant.
Other signs of optic neuropathy include clouding or darkening of vision for a few seconds, which then resolves. This sudden and short change in vision is called a transient ischemic attack, which can indicate that there is a potential issue with the blood flow to your optic nerve. You may suffer vision damage if you ignore this symptom, and you may have blood flow problems in other parts of your body, including to your brain.
While there are several potential causes of optic neuropathy, some of the most common symptoms include:
- Pain in the eyes.
- Loss of peripheral vision, or the sides of the visual field.
- Loss of color vision.
- Flashing lights called
- Loss of sight in one eye but not the other.
- Double vision.
- Pain in the eye socket or face.
Problems That Can Cause Optic Neuropathy

Almost any underlying, chronic condition, injury, or toxin can lead to nerve damage in the eyes. It is important to know what your risks are, so if you begin to experience changes to your vision, you can visit your eye doctor immediately and discuss the potential causes of your vision issues.
- Chronic relapsing inflammatory optic neuropathy: While this is a rare condition, a side effect of preexisting eye damage or inflammatory conditions can become optic neuropathy over time. One case study reported that an individual with asthma, migraines, and a family history of ocular sarcoidosis and lupus in close relatives reported painful loss of vision in the left eye. Attacks occurred frequently, but they were temporary. There was no involvement in the right eye, but other physical symptoms occurred when loss of left eye vision occurred. These were symptoms of ongoing damage to the optic nerve.
- Compressive and infiltrative optic neuropathy: This is compression of blood vessels in or around the optic nerve and retina caused by compression or invasion of other tissues, usually from another source like a tumor. Aneurysms, strokes, or severe injury can also cause infiltrative optic neuropathy.
- Disease and nutritional deficiency: Some diseases may cause optic neuropathy. For example, Dengue fever has had instances of optic neuropathy associated with the condition. The virus caused optic neuritis, which led to damage to the optic nerve. While this is rare, disease as a cause of optic nerve damage may be underreported. Diabetes and hypertension are diseases that are also associated with blood flow problems that cause nerve damage, including to the optic nerve. Addiction is a chronic medical condition that can contribute to nutritional deficiency, making optic neuropathy worse. Anorexia nervosa, anemia, gastrointestinal disease, pathogens, kidney failure, and metabolic disorders may also contribute to nutritional deficiency associated with optic nerve damage. Diagnosing these conditions should involve a review of overall physical health to look for gait problems, sensory disturbances, and changes to touch sensitivity in the extremities. Loss of vitamin B12, or thiamine, is the most common source of nutritional optic neuropathy. This condition is often caused by an underlying disease.
- Heredity: There are some genetic conditions that lead to optic nerve degradation, congenitally or over time. These include:
- Leber’s hereditary optic neuropathy (LHON).
- Dominant optic atrophy.
- Behr syndrome.
- Berk-Tabatznik syndrome.
- Ischemic optic neuropathy: One of the more common forms of optic neuropathy, this condition is caused by insufficient blood flow to the optic nerve, leading to tissue damage and death. There are two parts of the optic nerve: the anterior and the retrobulbar. The anterior section is supplied with blood from the short posterior ciliary artery and choroidal circulation. The retrobulbar optic nerve gets blood flow from pial plexus, which comes from a cluster of other arteries. Ischemic optic neuropathy is classified based on where the cut-off blood flow comes from.
- Anterior ischemic: Diseases or injury causes harm to the head of the optic nerve, leading to swelling of the optic disc.
- Posterior ischemic: There is no disc swelling at first, but there is a subsequent development of optic atrophy due to lack of blood from posterior blood supplies, often associated with sudden loss of vision.
- Radiation: This form of optic atrophy occurs due to changes in blood supply caused by radiation treatment, such as those for cancer. This damage to the optic nerve from loss of blood flow may occur three to eight months after treatment.
- Medication for hepatitis C: Changes to blood flow caused by interferon or other treatments for hepatitis C may lead to damage to the optic nerve.
- Optic neuritis: This is inflammation that can, at its most extreme, damage the optic nerve and lead to vision loss. Pain and temporary loss of vision in one or both eyes can suggest that optic neuritis is beginning. It is also one of the symptoms of multiple sclerosis (MS), a progressive, chronic condition that leads to nerve damage, including in the spinal cord and the brain. Optic neuritis may be one of the first signs of MS, or it could occur later as the disease progresses. This type of nerve damage has also been associated with autoimmune disorders (particularly lupus), which can cause inflammation that damages the optic nerve. Some causes of optic neuritis can be managed with medicated eye drops, but most require overall medical treatment, as the optic nerve damage is a symptom of a larger disease.
- Toxic neuropathy: Drug abuse or toxic chemicals in the environment can lead to damage to the optic nerve. Drugs; metals like lead, mercury, and thallium; organic solvents including ethylene glycol and toluene; carbon dioxide; methanol; and cigarette smoke can all damage the optic nerve. Unlike some forms of optic neuropathy, toxic causes are likely to lead to bilateral loss of vision. The problem may be triggered or enhanced by nutritional deficiencies, particularly associated with substance abuse or drug addiction.

Optic Neuropathy Treatment Usually Involves Addressing Underlying Conditions
If you develop any symptoms of optic neuropathy, you need to see an ophthalmologist immediately. You may also benefit from working with your general practitioner on potential underlying diseases or health risks that may have led to damage to your sight.
Your ophthalmologist and/or GP may refer you to a neuro-ophthalmologist who can test the connection between your optic nerve and your brain. They can diagnose the severity of the damage and how to best treat the underlying cause.
It is important to know that your visual acuity, or the sharpness of your vision as tested by the Snellen chart, may not be affected. Normal annual eye exams may not detect damage to the optic nerve unless there is associated damage to the retina. This is why it is important to report any symptoms you experience as soon as possible.
Treatment for optic neuropathy may slow down the progression of damage, but you will not regain the sight you lost. If you struggle with an underlying medical condition, diagnosing and treating that will reduce harm to your sight.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
References
- Optic Neuropathy. (2009) The Free Dictionary, Medical Dictionary.
- Clinical Approaches to Optic Neuropathies. (September 2007). Clinical Ophthalmology.
- Chronic Relapsing Inflammatory Optic Neuropathy. (April 9, 2018). Neurology.
- Dengue Optic Neuropathy. (January 2009). Ophthalmology Journal, American Academy of Ophthalmology (AAO).
- Toxic Optic Neuropathies: An Updated Review. (2015). Acta Ophthalmologia.
- Hereditary Optic Neuropathies. (2004). Nature: Eye.
- What Is Ischemic Optic Neuropathy? (April 25, 2018). American Academy of Ophthalmology (AAO).
- Anterior Ischemic Optic Neuropathy (AION). (May 9, 2017). Medscape.
- Optic Neuritis. (November 4, 2016). Mayo Clinic.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.