Cystoid Macular Edema (Macular Degeneration): Symptoms and Treatment
Last Updated:
Table of Contents
Cystoid macular edema refers to swelling in and below the delicate tissues that lie in the back of the eye. These tissues are responsible for our ability to see fine detail in the center of the visual field, and when they are damaged, reading, driving, and computer work can all be difficult to complete.
This is a form of macular degeneration, and it takes hold when the natural balance of fluid and pressure in the eye is disrupted. This condition can develop due to an underlying health problem, such as diabetes, or it can develop after eye surgery.
Since the symptoms of this form of macular degeneration can be similar to other forms of macular degeneration, it’s important to get a diagnosis from a doctor, so treatment can begin.
Cystoid macular edema can be treated with medications as well as some forms of surgery. With the right therapy, many people do see improvement, although it can take time.
How Cystoid Macular Edema Takes Hold
The eye is a remarkably delicate piece of anatomy, and in order to function properly, the eyes need to keep layers separate but equal. As the American Academy of Ophthalmology explains, each part of the eye must be nourished with fluid, and that fluid level must be regulated. When the eye is working properly, fluid moves into the eye at the same rate it is removed from the eye. That allows all tissues to get the nourishment they need without growing, so no layer pushes another out of place.
For people with cystoid macular edema, this process breaks down. Fluid begins to collect both within the macular tissue and beneath it. As the tissue swells with fluid, it begins to change in shape and size. Other parts of the eye are compressed as this macular tissue swells, and even that growing pressure does not push the extra fluid out.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
As the macula changes in size, it becomes less able to transmit accurate images to the vision center within the brain. Instead, the images it sends along are distorted in direct proportion to the damage done. The more swelling, the more visual disturbance the person might experience.
According to the American Academy of Ophthalmology, people with cystoid macular edema have vision that looks like a picture that might emerge on an older television set. The overall picture might be blurry, and the colors within that image might appear washed out or not vivid.
It is worth noting that the severity of the symptoms can vary. Some people may experience holes in vision, while others may experience only a softening and blurring of most images.
Cystoid Macular Edema Causes
Chief among the reasons someone may develop cystoid macular edema are diabetes, unveitis, macular degeneration and certain vein blockages.
Diabetes
Diabetes is one of the most common causes of cystoid macular edema. Uncontrolled or chronic diabetes (type II) can affect peripheral blood vessels in your retina. Cystoid macular edema occurs when blood vessels in the eyes leak blood, fluid and sometimes fat.
Uveitis
Uveitis refers to the inflammation of the uvea, the pigmented middle layer of your eye that lies between your inner retina and the fibrous outer layer comprising of your cornea and sclera. Intermediate uveitis and chronic uveitis may cause macular edema.
Macular Degeneration
Macular degeneration because of aging can also cause cystoid macular edema. The natural deterioration of your macula that occurs when you age may be characterized by yellow deposits (drusen) under your retina. Sometimes, this deposition is accompanied by abnormal blood vessel formation that may result in macular edema.
Vein Blockage
High blood pressure, atherosclerosis and glaucoma can cause vein blockage in your retina. These specific conditions cause nearby retinal veins to become engorged and thus leak fluid into or under your retina, characteristic of cystoid macular edema.
Risk Factors for Cystoid Macular Edema
Almost every single part of the human body can swell, and often, swelling happens due to an injury. When the body is attempting to heal, it swells in order to protect the tissues and keep the damage from spreading. Sometimes, swelling happens after damage that happens in surgery.
During a surgical procedure, doctors make small incisions. They remove tissue or insert lenses to fix an underlying problem. All of those steps can seem like injuries to the body, and swelling can take hold in return.
A common surgery performed to the eye involves cataract surgery. Here, doctors remove the crystalline lens within the eye that has been clouded with cataract, and they replace that damaged lens with a new one. The cuts are small, and often, these surgeries happen without a problem. But sometimes, cystoid macular edema happens after cataract surgery.
According to an article published in Clinical Ophthalmology, about 20 percent of people who have cataract surgery develop cystoid macular edema after surgery. Some have the issue right after surgery, but others do not develop the issue until months or even years later.
In addition to surgery, there are other risk factors for macular edema, according to the American Society of Retina Specialists.
- Diabetes
- Blood vessel disease
- Macular disease, including age-related macular degeneration
- Eye tumors
This highlights just how many conditions could play a role when macular edema takes hold.
How Your Doctor Diagnoses the Problem
People who experience symptoms of cystoid macular edema are encouraged to visit a doctor as soon as possible. Doctors can perform a variety of tests to determine what is causing the vision changes, and with a diagnosis in place, doctors can figure out what treatment steps should come next.
According to the National Eye Institute, a doctor moves through a step-by-step exam to diagnose macular edema. Your doctor might start by testing your visual acuity, or how well you can see. This is a test you might be familiar with, as it involves covering an eye and reading letters and numbers on a board. Your doctor might also place drops in your eyes, in order to make your pupils large. Those large pupils will allow your doctor to see the retina at the back of the eye.
Your doctor may also perform a fluorescein angiogram. In this test, a small amount of dye is placed in your arm, and a special camera takes pictures of the inside of your eye as the dye moves through blood vessels. Your doctor may also use a special light and a camera to measure the thickness of your retina.
These tests should not cause any pain or discomfort, and they can give your doctor a great deal of information about what is happening deep within your eye. With a formal diagnosis of cystoid macular edema, your doctor can determine what treatment steps are right for you.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Treating Cystoid Macular Edema
The goal of a treatment program for cystoid macular edema is to remove excess fluid from the eye. The program may also help the macula to return to a flat shape at the back of the eye, so normal vision can be restored.
Treatments can start immediately, but they can take time to work. According to an expert quoted by the Foundation Fighting Blindness, doctors hope to see improvement within about two months of beginning treatment, although it can take up to four months for some people to see real healing.
Doctors can use injections deep into the eyeball to help with cystoid macular edema. In this treatment, doctors load up a very thin needle with drugs that shrink or close blood vessels. Those drugs can help to stop the rapid movement of fluid from the bloodstream into the macula, and the drugs can therefore help the swelling to go down.
Doctors can also use steroids to reduce swelling, and those drugs can be given via needles placed within the eye. Some doctors use eye drops with steroids or muscular injections of steroids instead.
The American Academy of Ophthalmology reports that some doctors use laser treatments to help people with cystoid macular edema. In this form of treatment, a doctor uses laser pulses to seal blood vessels and stop fluid from leaking into the macula. The surgery takes just minutes to perform, and patients should feel no pain during the procedure.
Doctors may also use a specialized form of surgery, known as a vitrectomy, to help patients heal. In this procedure, according to the American Society of Retina Specialists, doctors use very small needles to remove a bit of the gel that sits inside of the eyeball. When this tissue is removed, pressure within the eye is eased, and the retina may be able to sit in the proper position. This procedure is often used in conjunction with another therapy, as it can rarely cure a problem alone. But it could be part of a treatment program for some people with cystoid macular edema.
Since cystoid macular edema can be caused by underlying health conditions, such as diabetes, your doctor will also want you to get treatment for your overall health. Leaving those conditions in place could mean allowing the problem to come back again. Working with a team to improve those conditions, so your eyes are healthier, is a wise step to take.
Is This the Same as Macular Degeneration?
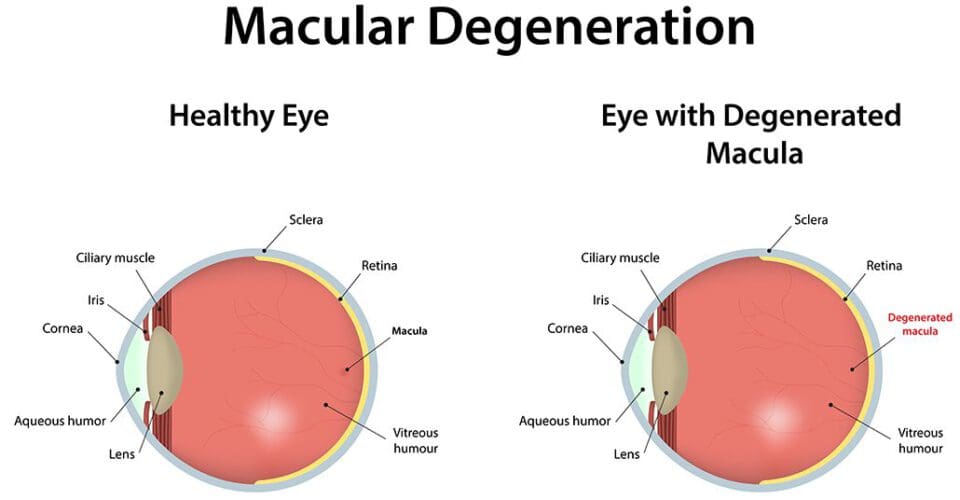
There are many forms of macular degeneration, including some that cause permanent loss of vision and others that are associated with advancing age. All of these conditions involve damage to the retina, so they all come with the label macular degeneration. But this condition is different, in that it is associated with swelling and fluid retention within the macula. No other form of macular degeneration comes with a swelling component like this.
In dry age-related macular degeneration, deposits sitting beneath the macula cause the tissue to buckle and bend, and that causes macular destruction and vision loss. In wet macular degeneration, abnormal blood vessels grow and burst beneath the macula, and this causes vision loss. These are totally separate conditions with different treatment programs.
That is why it is so important for you to see a doctor when you experience changes in your vision. Your doctor can examine your eyes and determine what is causing your symptoms. They can then provide the right therapy for those conditions, so you have the best chance of getting better quickly. You should never guess when your vision changes. You should always see an expert.
We can help. At NVISION, we specialize in helping people to protect and preserve their vision. We can offer surgical solutions for some types of issues as well as comprehensive medical care and monitoring for others. Our doctors are ready and willing to help you with your eyes. Contact us to set up an appointment.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
References
- Cystoid Macular Edema. (December 2014). American Academy of Ophthalmology.
- What Is Macular Edema? (August 2018). American Academy of Ophthalmology.
- Cystoid Macular Edema. (December 2008). Clinical Ophthalmology.
- Macular Edema. (2016). The American Society of Retina Specialists.
- Facts About Macular Edema. (October 2015). National Eye Institute.
- CME—What It Is, and Why People With Retinal Diseases Should Know About It. (February 2015). Foundation Fighting Blindness.
- Macular Edema Treatment. (August 2018). American Academy of Ophthalmology.
- Vitrectomy. (2016). The American Society of Retina Specialists.
- What Causes Macular Edema? (October 2020). American Academy of Ophthalmology. Date fetched: November 12, 2021.
- Overview: Uveitis (January 2020). National Health Service. Date fetched: November 12, 2021.
- Etiology and treatment of the inflammatory causes of cystoid macular edema (October 2009). Journal of Inflammation Research.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.

