What Is Tunnel Vision, and Can It Be Fixed or Prevented?
Home / Eye Conditions & Eye Diseases /
Last Updated:
What Is Tunnel Vision?

People with normal peripheral vision have a lateral field of view that creates an almost 180-degree angle and vertical field of view of about 135 degrees. This sight span usually lets someone see things that are to the far right and the far left.
Tunnel vision describes a condition in which that vision field is much more reduced, and it refers to cases when peripheral vision is moderately or severely restricted. Moderate and severe cases of side vision problems can lead to peripheral vision loss, creating the sensation of looking through a narrow tube. This is called tunnel vision.
Leading causes are glaucoma and retinitis pigmentosa. If tunnel vision is caught in an early stage, multiple treatment options are available, from medications to laser therapy to surgery.
A person can have peripheral vision problems even if they have excellent central, or straight-ahead, vision.
Table of Contents
Causes of Tunnel Vision
Glaucoma, a collection of diseases that harm the eye’s optic nerve, causes peripheral vision loss. It is one of the most common causes of tunnel vision.
Another leading cause of tunnel vision is retinitis pigmentosa, a rare and inherited eye disease that’s currently untreatable and leads to blindness.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
Some people experience tunnel vision when they’re under extreme stress or experiencing an anxiety disorder.
Because many of the conditions that cause tunnel vision have no early symptoms and can cause irreversible vision loss, early detection is important for prevention. A healthy lifestyle and diet can also promote eye health.
Other Causes of Tunnel Vision
Any condition that causes peripheral vision loss or degeneration of eye health can result in tunnel vision. This includes:
- Eye strokes or occlusions
- Detached retina
- Brain damage from stroke or injury
- Neurological damage
- Compressed optic nerve head
- Head injury or concussion
- Age-related macular degeneration (AMD)
Glaucoma and Tunnel Vision
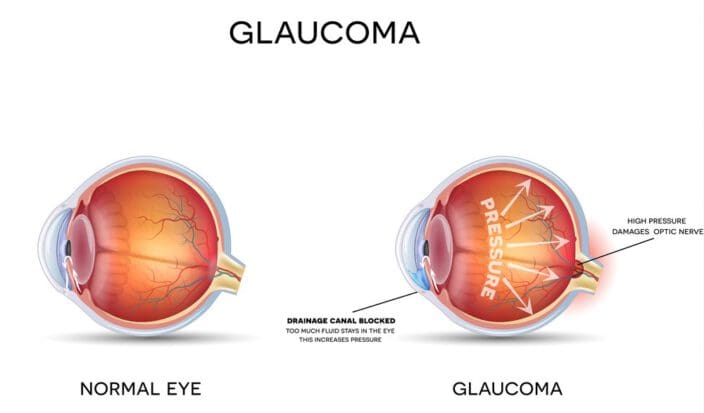
Glaucoma is a group of diseases that damage the eye’s optic nerve, which is a bundle of nerve cells that transmit messages from the eye to the brain. Although the optic nerve is part of the eye, it functions as a component in the central nervous system.
Glaucoma is caused by high pressure in the fluid inside the eye (vitreous fluid), which compresses the optic nerve, resulting in cell damage.
The damage from glaucoma usually begins with peripheral vision loss, which is why many people don’t realize they have glaucoma until the disease has advanced and created a peripheral field defect. A person’s central vision may be excellent, and they may not realize that they’re missing objects in their side vision until significant damage to their vision has already occurred, and they have tunnel vision.
There is no cure for glaucoma, and any loss as a result of glaucoma is irreversible. However, if caught early, medicine and surgery (laser and conventional) can halt the progress of the disease and prevent further vision loss.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
Retinitis Pigmentosa
Retinitis pigmentosa (RP) is a rare disease that is inherited and currently untreatable. The disease causes the retina to slowly and progressively degenerate.
Symptoms of retinitis pigmentosa usually start in childhood, but the disease isn’t likely to develop in an individual until they are in their 20s or 40s, depending on genetics.
The disease and its progression are unpredictable. In early stages of RP, light-sensing cells may begin to deteriorate, making night driving more difficult. The field of vision may begin to narrow, sometimes creating a tunnel vision effect.
In advanced stages of RP, only a small area of central vision and slight peripheral vision may remain. This may feel like extreme tunnel vision.
Although there’s currently no cure or effective treatment for RP, research is ongoing. Occupational therapy at the beginning phases of RP can be helpful for managing the transition into the more advanced phases of the disease.
Stress and Tunnel Vision

Individuals under high levels of stress and those who struggle with anxiety disorders, like post-traumatic stress disorder or social anxiety disorder, may experience tunnel vision as a symptom of their fear or anxiety, along with other symptoms like increased heart rate, muscle tension, sweating, and shortness of breath. This type of tunnel vision is short term, as vision will return to normal as the anxiety subsides.
New research suggests that stress can lead to other, more long-term eye and vision problems, including glaucoma, diabetic retinopathy, and optic neuropathy. There is even some research suggesting that a reduction in stress may help to restore damaged eyesight, although this has not yet been fully proven.
Treatments for Tunnel Vision
Treatment for tunnel vision typically follows the same process regardless of how advanced the condition. Doctors like to start with prescription medication. Next comes an option of laser therapy or else a combination of laser therapy and meds.
The last treatment option is surgery.
Medications
Doctors have a variety of prescription medicines at their disposal to help lower IOP. The drugs fit into five different categories based on what they do.
- Prostaglandin analogues: These are the most common drugs, and more than half of patients take them. They improve the flow of aqueous humor out of the eye through the non-conventional pathway.
- Beta adrenergic blockers: They reduce the production of aqueous humor. About 25% of patients take these.
- Alpha 2 adrenergic agonists: These have a combination effect, reducing secretion of aqueous humor while also improving aqueous humor flow.
- Carbonic anhydrase inhibitors: These reduce secretions. Pills have shown to be more effective than drops or creams.
- Cholinergic agonists: These increase aqueous draining through conventional pathways.
Patients often take two or more drugs to improve their sight before doctors recommend laser therapy or surgery.
Laser Therapy
People whose vision does not improve through drug therapy are candidates for one of two types of laser therapy—laser trabeculoplasty or laser diode cyclophotocoagulation.
Laser trabeculoplasty serves as the primary treatment. Laser diode cyclophotocoagulation is a rare procedure and typically not used in POAG.
Surgery
If laser therapies don’t fix the vision, surgery is the next, and last, option. There are three possible procedures: trabeculectomy, glaucoma implant surgery or minimally invasive glaucoma surgery (MIGS).
Trabeculectomy
This procedure is usually performed in a hospital or surgery center. A surgeon makes a small opening in a spot at the top of the eye that is usually covered by the eyelid. This permits for extra fluid drainage and lessening the pressure in the eye.
Glaucoma Implant Surgery
Used to treat various types of glaucoma, this surgery is performed at the hospital or surgery center, too. The surgeon places a small shunt in the white of the eye, creating a new drain for excess eye fluid.
Minimally Invasive Glaucoma Surgery
Doctors turn to this option for mild cases of glaucoma, and there are multiple procedures they can perform: Microtrabeculectomies, trabecular surgery, suprachoroidal shunts or newer laser procedures.
- Microtrabeculectomies: Microscopic tubes are inserted into the eye to enable draining under the outer eye membrane. Technological advances in shunt development make these procedures more successful
- Trabecular surgery: In this procedure, the surgeon bypasses or eliminates the trabecular meshwork that traps excess fluid.
- Suprachoroidal shunts: The surgeon connects the suprachoroidal space (between the retina and the eye wall) to the front of the eye to add extra drainage. Patients experience few complications, and shunts often can help drain a substantial amount of fluid.
- Newer laser surgeries: Recent advancements in laser technology have surgeons looking at these procedures more, usually for patients whose glaucoma is not severe.
Preventing Tunnel Vision
Because many of the conditions that cause tunnel vision are hard to detect, and treatment for them is much more effective in early stages of development, early detection is the most important step in preventing tunnel vision. Thorough annual visual exams should be part of everyone’s health routine.
This is especially important for people who are prone to diseases that cause tunnel vision, including individuals who:
- Have a family history of glaucoma or retinitis pigmentosa.
- Are African American or Latino.
- Have diabetes, heart problems, or high blood pressure.
- Are experiencing vision loss due to age or any other condition.
- Have had a head injury or stroke.
- Have anxiety disorders or are under extreme stress.
- Experience poor night vision.
- Have noticed they have blind spots in their vision.

Genetics and family vision history can play a significant factor in eye health and vision. Overall health also has an impact, and good health can help to prevent tunnel vision and other damaging eye conditions. Beneficial levels of exercise and movement can improve blood pressure and stress levels, preventing health problems like eye disease.
Diet can also help to prevent tunnel vision and vision loss. Certain vitamins and nutrients — like antioxidants, omega-3 fatty acids, zinc, and phytochemicals — may promote eye health and strong vision. Foods rich in these nutrients, like kale, eggs, nuts, and oily fish, may be helpful.
Conversely, unhealthy foods, including refined carbohydrates and highly processed junk foods, may contribute to poor eye health. They should be avoided by those looking to prevent or halt the development of eye disease.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
References
- Peripheral Vision Loss (Tunnel Vision): Causes and Treatments. (January 2017). All About Vision.
- What Are the Symptoms of Glaucoma? (October 29, 2017) Glaucoma.org.
- Retinitis Pigmentosa. (September 2016). All About Vision.
- The Positive Side to Your Anxiety. (September 24, 208). Verywell Mind.
- Persistent Stress May Lead to Vision Loss, Study Shows. (June 21, 2018). Medical News Today.
- Mental Stress as Consequence and Cause of Vision Loss: The Dawn pf Psychosomatic Ophthalmology for Preventative and Personalized Medicine. (June 2018). EPMA Journal.
- Tunnel Vision – Loss of Peripheral Vision. (November 2, 2018). Verywell Health.
- Top 10 Foods for Healthy Eyes. (March 17, 2018). Medical News Today.
- Junk Food May Be Bad for Your Eyesight. 2001. American Macular Degeneration Foundation.
- Tunnel Vision: The Economic Impact of Primary Open Angle Glaucoma – A Dynamic Economic Model. (February 2008). Center for Eye Research Australia.
- What is MIGs? (June 23, 2020). Glaucoma Research Foundation.
- Glaucoma Surgery. (June 26, 2019). National Eye Institute.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.