Eye Herpes: Causes, Treatment & What Not to Do
Home / Eye Conditions & Eye Diseases /
Last Updated:
What Is Eye Herpes?
There are two common types of herpes virus – herpes simplex virus I (HSV-1), also called oral herpes, and herpes simplex virus 2 (HSV-2), which is genital herpes. These two forms of the herpes virus can spread to other parts of the body and cause lesions or sores. One area they spread to is the eyes, leading to epithelial keratitis, viral keratitis, herpes keratitis, or eye herpes.
Typically, eye herpes comes from HSV-1, transmitted when a person touches a cold sore on their lip and then touches their eye. However, epithelial keratitis can also stem from HSV-2.
Eye herpes can be controlled with antiviral medication, and it can be diagnosed during a routine eye exam. However, untreated eye herpes can damage deeper layers of the eye and eventually cause blindness.
When HSV infects the eye, the infection hits the cornea first. This is the clear dome over the pupil, which is involved in refracting light onto the retina. Herpes never fully goes away, but most instances of herpes keratitis heal on their own, just like cold sore outbreaks. Severe forms can cause blindness if they are not treated.
Table of Contents
Eye herpes comes from one of two common types of herpes virus, typically herpes simplex I (HSV-1). This condition may be called epithelial keratitis, viral keratitis, or herpes keratitis.
Symptoms include redness, pain, eyelid swelling, or discharge from the eye. These symptoms resemble conjunctivitis, but if they recur within a year, you may have a virus rather than bacterial or chemical exposure.
It is important to get a diagnosis from an optometrist or ophthalmologist so you can follow a treatment plan to suppress the virus. If you don’t, future outbreaks could move further into the cornea or iris, causing stromal keratitis or iridocyclitis, both of which can lead to blindness.
Avoid touching your eyes or sharing eye products if you have cold sores or know someone with eye herpes. Take any eye drops or oral medications as prescribed to manage the herpes virus.
Causes & Symptoms of Eye Herpes

Keratitis, or inflammation or infection of the eyes, has several potential causes, including bacteria, parasites, overexposure to ultraviolet (UV) light, or a virus (specifically HSV-1 or HSV-2).
There are roughly 20,000 new reported cases of eye herpes in the United States every year, with 48,000 total reported infectious episodes.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
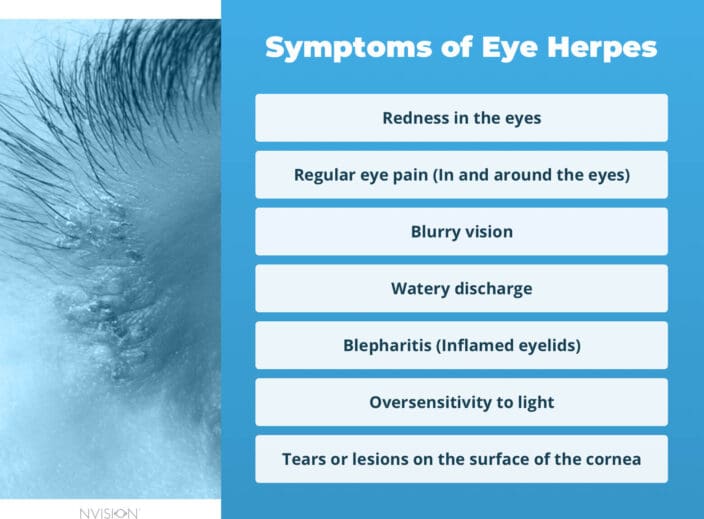
Herpes keratitis symptoms often are misdiagnosed or even dismissed as something else. It’s important to remain vigilant and consult your medical service provider if you experience symptoms that mirror those of eye herpes, such as:
- Redness in the eyes
- Regular eye pain
- Blurry vision
- Watery discharge
- Blepharitis (inflamed eyelids)
- Oversensitivity to light
Contact lenses increase your chance of infection and re-infection. If you’re diagnosed with eye herpes and wear contact lenses, you should discard them and get new ones. Moreover, you can discuss other corrective measures with your ophthalmologist.
With any type of herpes virus that affects humans, the virus can enter the body and remain dormant for years. Forms of physical or emotional stress typically lead to the virus becoming active, either for the first time or as a flareup. Common causes of flareups include:
- Emotional or mental stress.
- Fever.
- Physical trauma to the body, like an injury or surgery.
- Exposure to UV light, including being outdoors or in a tanning bed.
- Menstruation.
- Some medications.
Mild or moderate symptoms from eye herpes can cause issues that are frequently mistaken for conjunctivitis. These health problems include:
- Red, watery, irritated eyes.
- Inflammation on the eyes and eyelids.
- Pain in and around the eyes.
- Tears or lesions on the surface of the cornea.

Conjunctivitis is an inflammation and infection of the sclera, the white part of the eye. It is caused by exposure to chemicals or toxins, allergies, or bacteria.
If your optometrist or ophthalmologist is unsure whether you have conjunctivitis or eye herpes, they will use a lab test to make a conclusive diagnosis. This is important, as treating these conditions helps you maintain healthy eyes and clear vision, but the treatment plans are different.
Children are most likely to contract eye herpes, usually in a mild form called keratoconjunctivitis. They will have red, perhaps itchy or watery eyes, until the flareup goes away. They may have another flareup that requires treatment from their eye doctor, but for the majority of children, one or two outbreaks is all they will experience. The herpes virus will remain dormant for the rest of their lives.
Treatment for Eye Herpes Suppresses the Virus
Getting an accurate diagnosis and appropriate treatment plan is important because severe forms of eye herpes can move into the stroma, a deeper layer of the cornea, and lead to stromal keratitis, which is harder to treat and can cause blindness. You may also develop iridocyclitis, when herpes infects the iris.
An optometrist or ophthalmologist will look at your eyes while your symptoms are active to make a diagnosis. Typically, lab testing is not necessary, but it can be performed in cases when the virus is less active, or symptoms are less clear.
If a lab test is needed, this will be a fluorescein eye stain. Your doctor will use an orange dye that fluoresces under certain light, and apply this stain to the surface of your eye, where the epithelial layer of your cornea is. This helps your doctor see any layers of scarring that may be from past herpes outbreaks.
Treatment for eye herpes is simple. Your doctor will prescribe eye drops or oral antiviral medications, which may be taken during outbreaks to suppress the virus and promote faster healing, or consistently for several years, depending on how severe and frequent outbreaks are when you are diagnosed. It is rare that eye herpes requires further treatment like surgery, but if outbreaks lead to scarring on your cornea or inside your eye, your eye doctor may recommend a laser procedure to remove scar tissue.
There is no cure for eye herpes once you contract it, but like other types of herpes virus, it is easy to manage symptoms and suppress the virus, so you rarely experience outbreaks. If you have stromal keratitis (the more severe, deeper type of eye herpes), you may receive anti-inflammatory steroid medications alongside antiviral drugs.
It is important to take medication as prescribed to reduce corneal scarring. This helps to maintain your vision. Repeated scarring and corneal perforation can require a keratoplasty, or corneal transplant, to treat.
Reduce Your Risk of Exposure to Eye Herpes

There are no clear ways to prevent the spread of herpes keratitis, but there are some steps you can take to keep your eyes safe.
- If you have cold sores, avoid touching your eyes. Wash your hands after you touch your lips during an outbreak to prevent spreading the virus to other areas.
- Do not share eye drops or eye makeup with others. The herpes virus can be transferred this way.
- Keep your contact lenses clean, as recommended by your optometrist. If you experience a herpes outbreak, throw out that pair of contacts.
If you are cautious, you can avoid transferring the virus to other areas of your body. It does take vigilance during outbreaks.
In the first year after contracting eye herpes, 20 percent of people will experience a recurrence of symptoms. If outbreaks become frequent, they can be managed with regular, often daily, medication. Otherwise, your doctor will prescribe medication that you will take only as needed, during your less frequent outbreaks.
For some people, the outbreaks are more frequent and more severe initially. Then, they stabilize over time and become less frequent.
While you may never need medication to treat eye herpes, it is important to get an appropriate diagnosis if you experience the symptoms listed above. Having more than one outbreak puts you at risk for scarring inside your cornea and other parts of your eye, which can lead to serious vision loss over time.
Although the term eye herpes can seem frightening, it is a normal and manageable condition with an appropriate diagnosis and treatment plan. Most often, it doesn’t require extensive treatment and can be effectively managed, making it a nuisance at times rather than a debilitating condition.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- Basics of HSV (Herpes Simplex Virus) Keratitis. (April 2014). Center for Disease Control and Prevention (CDC).
- What Is Herpes Keratitis? (April 2018). American Academy of Ophthalmology (AAO).
- Herpes Simplex Keratitis. Merck Manual: Consumer Version.
- Eye Herpes (Ocular Herpes). (November 2017). All About Vision.
- Molecule halts herpes of the eye. (February 27, 2018). National Institutes of Health.
- Halting herpes eye disease. (July 2021). University of California-Irvine School of Medicine.
- Herpetic Eye Disease Study (HEDS) I. September 17, 2009). ClinicalTrials.gov.
- Herpetic Eye Disease Study (HEDS) II. (March 24, 2010). ClinicalTrials.gov.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.

