Eye Discharge? Causes and How to Stop It
Home / Eye Conditions & Eye Diseases /
Last Updated:
If you wake up with crustiness or goop around the edges of your eyes, this is normal. Everyone has this kind of discharge, or rheum, in the morning.
Table of Contents
If you notice changes in your eye discharge, it can indicate that your eye is infected or injured. This might be a very serious issue requiring immediate medical attention.
To prevent infections and safely manage normal discharge, follow these steps:

- Keep your hands clean.
- Do not pick at your eyes.
- Keep eyes hydrated with artificial tears, as needed.
- Wipe away eye discharge from sleep with a clean, damp cloth.
Your eye discharge can be an indicator of your eye health. Do not hesitate to seek treatment if there are changes or other symptoms.
What Is Eye Discharge? Is it Normal?
Everyone has discharge from their eyes in the form of “sleep,” mucus, sand, rheum, or a sludgy substance that is present in the corners of your eyes and on your eyelashes when you wake up. This discharge is a collection of tears, oil, skin cells, and debris that accumulates in and around your eyes as you sleep.

Because you do not blink tears, and the detritus they collect, out of your eyes while you are asleep, this mixture collects near the tear ducts. When you wake up, you have some crust or goopy areas, which can be easily brushed away. This substance is often white, off-white, or slightly yellow in tint.
There are some kinds of eye discharge that indicate a more serious condition. If your morning eye discharge turns yellow or green, you may have an infection. If your eyes discharge more substance than normal, this may indicate problems with your eyes. Discharge during the day, while you are awake, is often a sign of a more serious condition.
Eye Discharge May Have a Medical Cause That Requires Treatment
Generally, some rheum or “sleep” that has collected around your eyes, eyelids, and eyelashes is fine when you wake up. However, if you wake up with different-colored rheum, blurry vision, light sensitivity, or pain in your eyes, this may indicate an eye infection or another serious eye condition, which is also producing discharge.
Some causes of eye discharge that need treatment include:
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
- Contact lenses. Even if you do not have an infection from wearing your contact lenses too long, simply wearing them for several hours may irritate or inflame your eyes. This can lead to more eye discharge than normal when you wake up in the morning.Do not sleep in your contact lenses unless your optometrist recommends a gas-permeable variety that is okay to sleep in. If you experience a lot more rheum in the morning, even when you do not have your contact lenses in, you may want to switch to daily disposable lenses.
- Chronic dry eyes. There are several potential causes of dry eyes, but the condition may lead to sluggish or thick tears, which can increase the amount of “sleep” collected around your eyes and eyelashes in the morning. Ask your optometrist about the best ways to treat chronic dry eye. A short-term or additional course of treatment may include over-the-counter saline eye drops.
- Allergies. Sometimes called allergic conjunctivitis, allergies triggered by plants, animals, or dust can cause watering in the eyes, redness, itching, and eye discharge. This may affect one or both eyes, and rheum is typically not an abnormal color. Antihistamines, eye drops, or other allergy treatments can manage this side effect.
- Conjunctivitis. An eye infection known as pink eye, conjunctivitis is accompanied by redness, swelling, pain, itching, or the feeling of grit in one or both eyes. Without treatment, this infection can spread and may even lead to eye damage. It is important to get a diagnosis from an optometrist and follow their course of treatment, which usually starts with medicated eye drops.
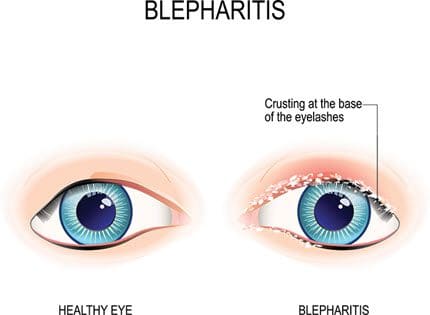
- Blepharitis. An inflammation of the eyelash hairs leading to swelling and pain around the eye can also cause discharge because of abnormal oil production around the follicles. Meibomian gland dysfunction (MGD) is sometimes associated with blepharitis, which can cause foamy eye discharge, crusting on the eyelids, and yellow or green pus from the eyes.
- Keratitis. There are several types of keratitis: bacterial, fungal, amoebic, photo, and herpetic. Bacterial keratitis is a corneal infection that develops quickly, and if left untreated, it can cause blindness. Excessive discharge that is an unusual color is one sign of bacterial keratitis. Fungal keratitis also infects the cornea, and it has similar symptoms as bacterial keratitis, but is caused by one of three types of fungus. Herpes keratitis is caused by a viral infection of herpes simplex, the same virus that causes cold sores (type I) or genital herpes (type II). Amoebic keratitis is an infection caused by an amoeba, usually acanthamoeba. Photokeratitis is caused by too much exposure to ultraviolet radiation, and it is a bit like a sunburn on the cornea.
- Stye. This is a clogged meibomian gland, usually at the base of the eyelid. These are typically infected eyelash follicles, which may require medical treatment, but they often go away on their own. Styes may look like pimples on the margin of the eyelid, and they can be painful or tender. Discomfort during blinking is also a sign of a stye, along with some extra discharge.
- Eye injury or trauma. Anything from cosmetics and perfume to being hit in the eye can cause injury or trauma to the structures of this organ. One sign that your eye is injured is excessive rheum or discharge. If this occurs while you are awake, looks more like pus, or contains blood, see an eye specialist immediately.
- Corneal ulcer. Sometimes, the cornea (the membrane over the top of the eye) becomes infected. This ulcerous spot can cause white discharge. Excessive tearing, pain in the eye, redness, trouble opening the eye, and sensitivity to light are all symptoms associated with corneal ulcers.Antibiotic treatment can get rid of this condition. If left untreated, corneal ulcers cause lasting damage and may lead to a corneal transplant.
- Dacryocystitis. This is a blocked tear duct, which can be quite painful. It will look like a tender, swollen lump under the inner eyelid. Water eyes, sticky eye discharge, redness, blurry vision, and pain are all associated symptoms. It may go away on its own, but speak with an ophthalmologist for an appropriate diagnosis.
Managing & Preventing Eye Discharge at Home
You may be tempted to rub or pick at your eyes in the morning to remove these clumps of discharge, but this can increase your risk of infection.
Sticking something in your eye accidentally can also lead to discharge. If you get cosmetics or dirt in your eye by accident, wash your eye out with water or saline drops. Do not wipe your eyes with your fingers.
Keep your hands clean. When you apply makeup, put in contact lenses, or rub your eyes because you are tired, you reduce your risk of getting an eye infection if your hands are clean.
If you are concerned about the discharge from your eyes, even in the morning, soak a clean washcloth or the corner of a clean towel in warm water. Then, wipe the area around your eyes, eyelids, and eyelashes. This removes the gunk and can also feel relaxing.
Is Eye Discharge Different in Babies and Adults?
Like adults, babies produce eye discharge, and this is normal.
Babies may sometimes produce excessive eye discharge due to a blocked tear duct. Since newborns’ tear ducts are not completely developed, they are more likely to get blocked. Apply a warm, soft compress to the baby’s eye and gently massage the area to loosen the blockage.
If the situation does not improve, or if the discharge is accompanied by redness or swelling, see a pediatrician. In rare cases, surgery may be needed to unclog a blocked tear duct.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
Changes in Eye Discharge Indicate Changes in Your Eye Health
A small amount of discharge, especially when you wake up, is normal for everyone’s eyes. However, if your discharge changes color, amount, consistency, or frequency, speak to an optometrist, especially if this does not stop after one or two days.
If eye discharge is accompanied by pain, redness, inflammation, changes to skin texture around your eye, trouble seeing clearly, or blood, see a medical professional immediately.
Sticky Eye
One of the most common causes of discharge in your baby’s eyes is called sticky eye. This will look like sticky discharge from one or both of your newborn’s eyes.
While discharge can be caused by an infection, sticky eye is not an infection. Instead, it typically occurs because newborns’ tear ducts are smaller and may become clogged in their first few days. As long as your child does not have redness in the whites of their eyes, puffiness or redness in the skin around their eyes, or an odd-colored discharge, there is likely nothing to worry about.
About one in five infants does not have fully formed tear ducts when they are born, making sticky eye the most common cause of discharge. Most pediatricians recommend that new parents wait a few weeks or months for the condition to clear up. Your pediatrician can also help you monitor sticky eye during your regular visits, so they can catch anything that might become a concern.
You can keep your child comfortable as sticky eye clears up with these tips:
- Wash your hands before and after you touch your child’s face.
- Wet a clean, soft cloth and gently wipe the area around their eyes.
- Alternatively, use a soft, damp cotton ball to gently wipe their eyes.
- If instructed by your pediatrician, you can gently massage your child’s tear duct area for a few minutes every day, putting pressure on either side of their nose.
- Return to your pediatrician for help if your baby reaches 12 months old and the condition has not cleared up.
Eye Infection
Another potential cause of eye discharge in your newborn or infant is an eye infection. The most common eye infection in babies is conjunctivitis, which is an inflammation of the thin outer layer of the eye, called the conjunctiva.
Symptoms of conjunctivitis are very similar to sticky eye, but the white of your child’s eye will appear pink or red. They may also have some swelling around their eyes, become fussier or cry more because of discomfort or pain, or reach up to rub their eyes (if they are old enough for this level of physical coordination).
Instead of a clear, sticky film, discharge from your baby’s eye will be clumpier and yellow. The discharge may start in one eye and then move to the other if the infection spreads.
You can also talk to your pediatrician about when your child will open their eyes for the first time. If they do not reach this milestone, there may be an underlying structural problem that needs to be addressed.
Treatment for Eye Discharge
Most cases of eye discharge don’t require treatment since some level of “sleep” or discharge is normal.
To effectively treat cases of eye discharge that are not normal, you’ll need to identify the underlying cause. See your eye doctor to assess what is causing your abnormal eye discharge. They’ll then prescribe the appropriate treatment.
For certain conditions, such as corneal ulcers and bacterial conjunctivitis, antibiotics may be needed. Other treatments may be prescribed as needed, according to the contributing issues.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
References
- Is That Morning “Eye Gunk” Normal? (January 3, 2018). University of Utah Health Center.
- What Causes Eye Boogers? (February 2, 2018). Medical News Today.
- Eye Discharge (Sleep in Your Eyes). (November 2016). All About Vision.
- What Is Bacterial Keratitis? (April 23, 2018). American Academy of Ophthalmology (AAO).
- What Is Fungal Keratitis? (December 5, 2018). American Academy of Ophthalmology (AAO).
- What Is Herpes Keratitis? (April 25, 2018). American Academy of Ophthalmology (AAO).
- Sticky Eye. (January 2015). Institute of Health Visiting (IHV), National Health Services (NHS).
- Eye – Pus or Discharge. (August 2020). Seattle Children’s Hospital.
- Conjunctivitis (Pink Eye) in Newborns. (January 2019). Centers for Disease Control and Prevention.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.