What Is a Coloboma? Can It Be Corrected?
Home / Eye Conditions & Eye Diseases /
Last Updated:
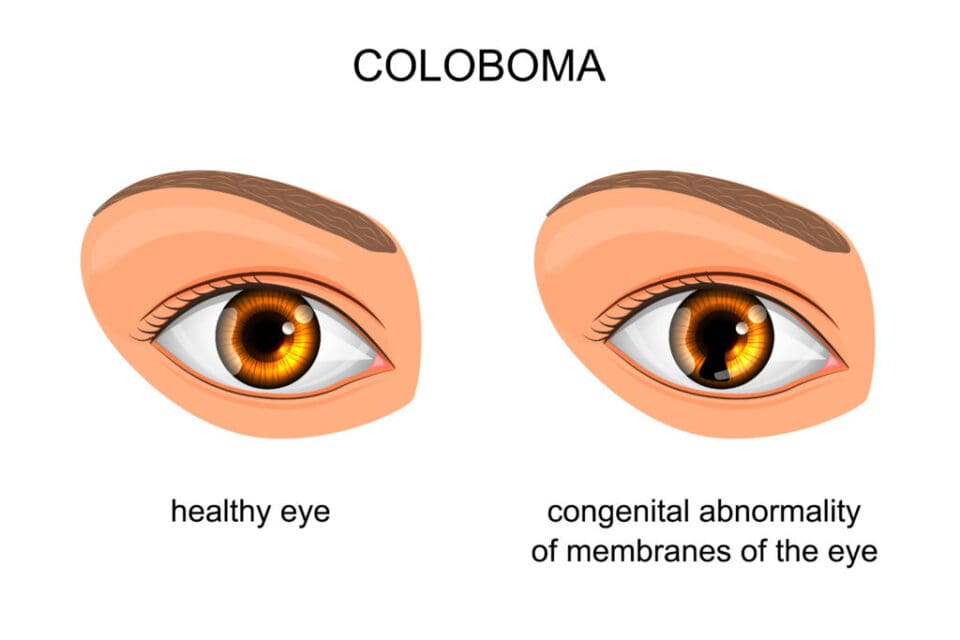
Coloboma is a condition that presents itself as a gap, or ‘missing piece’, in the structure of the eye. It arises when the eyes, which are formed around a central seam during fetal development, fail to close completely at around seven weeks of gestation. This anomaly may affect virtually any part of the eye, such as the iris, cornea, or even the eyelid.
While it’s true that coloboma is an uncorrectable condition, it’s equally important to remember that it’s manageable, especially with regular eye exams. These help medical professionals identify and mitigate potential complications, like glaucoma or retinal detachment, before they lead to more severe vision loss.
The experience of living with coloboma varies greatly, dependent on the location and size of the gap. For some, this can mean sun sensitivity and low vision. Yet, a range of adaptive strategies and lifestyle modifications can help individuals cope with these challenges.
What Is Coloboma?
Coloboma is a congenital eye condition that arises from an irregularity in the development of the eye during early stages of pregnancy. This condition results in missing or undeveloped tissue in one or more structures of the eye.
Though this irregularity can potentially occur in any part of the eye, its presence is most noticeable when it happens in the iris – the colored portion of the eye. Here, it can give the iris an extended or irregular shape, often compared to a keyhole. It’s also worth noting that coloboma can manifest in less visible parts of the eye, such as the retina or optic nerve.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Despite being present from birth, coloboma is non-progressive, meaning it doesn’t worsen over time. It can occur as an isolated condition or as part of a broader genetic condition. In the sections to follow, we will explore the various symptoms associated with coloboma, delve into its different types, understand who is at risk, and discuss available methods of diagnosis and treatment options.
Types of Coloboma
| Type | Location | Appearance/Effect | Impact on Vision |
|---|---|---|---|
| Iris Coloboma | Iris | Keyhole shape | Light sensitivity |
| Retinal Coloboma | Retina | Not visible to naked eye | Possible vision loss |
| Optic Nerve | Optic nerve | Not visible to naked eye | Vision loss in field |
| Eyelid Coloboma | Eyelid | Physical notch or defect | Cosmetic |
| Lens Coloboma | Lens | Not visible to naked eye | Blurred vision |
| Choroidal | Beneath retina | Not visible to naked eye | Similar to Retina |
Coloboma can affect various parts of the eye, each with its own characteristics and potential impacts on vision. The following are some of the most common types of coloboma:
- Iris Coloboma: Affects the colored part of the eye, giving it a keyhole appearance. It may lead to sensitivity to light but typically does not significantly impact vision.
- Retinal Coloboma: Occurs in the retina, which is responsible for processing light. It can lead to vision loss or blind spots, depending on the size and location of the missing tissue.
- Optic Nerve Coloboma: Affects the optic nerve that connects the eye to the brain. It can result in vision loss in one part of the visual field.
- Eyelid Coloboma: Affects the eyelid, leading to a physical notch or defect in the lid. It usually has cosmetic effects but can cause dryness or irritation.
- Lens Coloboma: Occurs in the lens of the eye and may affect focusing ability, leading to blurred vision.
- Choroidal Coloboma: Affects the choroid, a layer beneath the retina. It can cause vision issues similar to retinal coloboma.
Symptoms of Coloboma
Most often, coloboma is detected by a doctor in infancy. It isn’t common for it to be detected in adulthood, but coloboma that is identified in babies and children may continue into adulthood.
These are the primary symptoms of coloboma:
- Light sensitivity
- Poor or declining vision
- Misalignment of the eyes
- Defect in the iris
What Causes Coloboma?
During gestation, babies develop along a sort of fault line. Tissues grow on either side of that fissure, and at some point, they connect into a formed whole. The structures of the eye all develop this way, and when something interrupts the process, a hole remains. That hole is coloboma.
Coloboma is a genetic condition, and that means it can be passed from parents to children. Coloboma can also be part of a genetic syndrome that causes other changes, in addition to faults in eye structures.
Specific genes that have been identified to potentially cause coloboma include PAX6, SHH, MAF, and CHX10.
Children who develop these issues do so early in life, as researchers say that the fissure in developing babies should close between weeks five and seven of pregnancy. Once they emerge, they remain even as the baby grows bigger during the rest of the pregnancy.
These issues are relatively rare, and the Royal National Institute of Blind People says about 1 in 10,000 births involve a coloboma. But when they develop, they can be serious. Gaps in eye structure can lead to eye illnesses that cause pain, disability, or both.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
Coloboma Diagnosis
Diagnosing coloboma typically involves a comprehensive eye examination conducted by an eye care professional. During this examination, various parts of the eye are carefully evaluated for missing or undeveloped tissue, which is characteristic of coloboma. Specific attention is given to areas such as the iris, retina, and optic nerve. In some cases, further assessments, such as visual field testing or genetic counseling, may be required to understand the full scope of the condition. The diagnosis is essential for creating an individualized treatment and management plan, and regular follow-up appointments may be necessary to monitor any changes or complications.
Coloboma Treatment
Treatment for coloboma is primarily focused on managing the symptoms and preventing or addressing any related complications, as the missing or undeveloped tissue cannot be replaced or repaired. The approach to treatment varies based on the type of coloboma and its impact on vision or appearance. Below are some common treatments and interventions:
- Regular Monitoring: Regular eye exams are vital for all types of coloboma to detect any potential complications early, such as glaucoma or retinal detachment.
- Prescription Glasses or Contact Lenses: For some types of coloboma, such as lens coloboma, corrective lenses can help in managing blurred vision or focusing issues.
- Sunglasses or Protective Eyewear: Individuals with iris coloboma may experience light sensitivity. Sunglasses or tinted lenses can help manage this discomfort.
- Surgical Intervention: In cases of eyelid coloboma where appearance or physical discomfort is a concern, surgical repair may be an option to improve the appearance and function of the eyelid.
- Low Vision Aids: For those experiencing significant vision loss, especially from retinal or choroidal coloboma, low vision aids like magnifiers or screen readers can be beneficial.
- Therapeutic Support: Ongoing support from eye health professionals, occupational therapists, and other specialists can help individuals adapt to vision changes and lead a full, active life.
- Genetic Counseling: As coloboma may be part of a broader genetic condition, genetic counseling might be recommended to understand the underlying cause and potential risks to family members.
It’s important to recognize that coloboma treatment is highly individualized. A personalized treatment plan is usually developed by a team of eye care professionals, geneticists, and other specialists, considering the specific type, severity, and associated symptoms of coloboma in each case.
While there may not be a cure for coloboma, ongoing care, appropriate interventions, and supportive resources can greatly enhance the quality of life for individuals living with this condition. The goal is to maximize visual function, comfort, and appearance while minimizing potential complications. Collaboration between medical professionals and patients is key to achieving these objectives.
What Happens If My Child Has Coloboma?
The discovery that your child has coloboma can be concerning and may raise many questions about what to expect. Here’s a general outline of what might occur if your child is diagnosed with this condition:
- Assessment and Diagnosis: Comprehensive eye examinations will be conducted to determine the type and extent of coloboma. The child’s vision, eye appearance, and any related symptoms will be carefully assessed.
- Personalized Treatment Plan: Based on the diagnosis, a specialized team of eye care professionals will develop a personalized treatment plan. This may include regular eye exams, prescription glasses, or other supportive measures tailored to your child’s specific needs.
- Ongoing Monitoring: Regular follow-up appointments will be essential to monitor your child’s vision development and to catch any potential complications early. Adjustments to treatment will be made as needed.
- Educational Support: If the coloboma affects vision significantly, educational support may be provided to ensure that your child has access to necessary accommodations in the classroom.
- Social and Emotional Support: Understanding and managing a child’s emotional response to coloboma and any associated challenges is crucial. Support from mental health professionals, counselors, or support groups may be beneficial.
- Cosmetic Considerations: If the coloboma is visible, as in the case of iris or eyelid coloboma, discussions about cosmetic appearance and potential surgical interventions may arise, depending on age and individual preferences.
- Family Planning and Genetic Counseling: If the coloboma is suspected to be part of a genetic condition, family members may be encouraged to undergo genetic counseling. This can help in understanding the risk of coloboma in future siblings and offer support in family planning decisions.
- Collaborative Care Approach: Care for a child with coloboma often requires collaboration between ophthalmologists, optometrists, pediatricians, teachers, and family members. Open communication and cooperation are key to ensuring the child’s well-being.
- Promoting a Normal Life: Most children with coloboma lead normal, healthy lives with proper care and support. Focusing on their abilities and strengths, rather than limitations, promotes a positive outlook and helps in integrating them fully into daily activities and social environments.
It’s vital to remember that every child’s situation is unique, and the above points are general guidelines. Engaging with a dedicated team of professionals who understand your child’s specific condition will provide the best pathway for support and care, promoting not just physical well-being but also emotional growth and development.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust.
Your journey to better vision starts here.
References
- Facts About Uveal Coloboma. (June 2012). National Eye Institute.
- Who Is At Risk for a Coloboma? (April 2018). American Academy of Ophthalmology.
- Incidence, Ocular Findings, and Systemic Associations of Ocular Coloboma: A Population-Based Study. (January 2011). JAMA.
- Coloboma. Royal National Institute of Blind People.
- Coloboma Factsheet. (October 2018). Royal National Institute of Blind People.
- Coloboma. FamilyConnect.
- Coloboma. American Foundation for the Blind.
- ABCB6 Mutations Cause Ocular Coloboma. (January 2012). The American Journal of Human Genetics.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.

