Secondary Cataracts: Why They Happen and How to Treat Them
Last Updated:

Article At a Glance
During cataract surgery, your doctor removes your damaged lens and replaces it with a synthetic version. Your old cataract can’t come back, as the damaged tissues are removed. But a secondary cataract can form weeks or months later.
The clinical name for this condition Is posterior capsular opacification (PCO).
Table of Contents
What Is a Secondary Cataract?
Surgeons use tissues within your eye to hold your artificial lens in place. Sometimes, those tissues degrade after surgery and blur your vision.
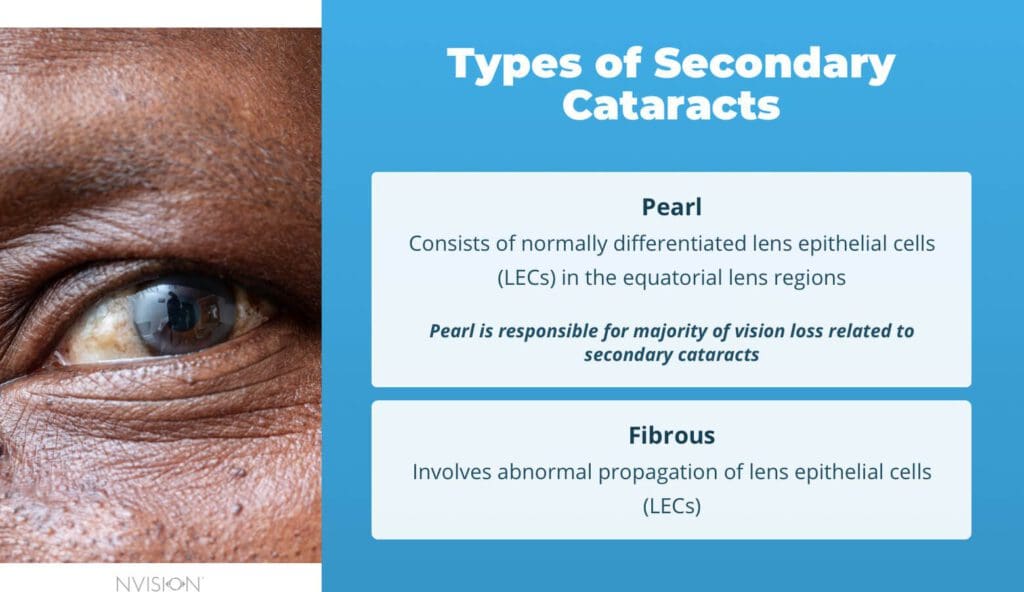

Your new lens sits within your eye’s natural lens capsule. Changes in that capsule can become cataracts. Two types of PCO exist:
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
- Pearl PCO consists of normally differentiated lens epithelial cells (LECs) in the equatorial lens regions
- Fibrous PCO involves abnormal propagation of LECs
A combination of these can be seen in some cases, but Pearl PCO is responsible for most vision loss related to secondary cataracts.
What Factors Increase the Risk of Secondary Cataracts?
Unfortunately, there is no way to know who will develop secondary cataracts after surgery or how long it will take for this condition to progress. But doctors are aware of some risk factors.
| Risk Factor | Description |
|---|---|
| Age | Younger people are at higher risk of secondary cataracts. |
| Illness | Conditions such as diabetes, uveitis, myotonic dystrophy, and retinitis pigmentosa slow down healing, which can encourage secondary cataracts to form. |
| Injury | If your cataract developed after a traumatic event, you could face secondary cataracts later. |
Your doctor’s surgical approach can help mitigate some of the risks:
- Lens selection: Square-edged lenses have been found to reduce the risk of PCO development, although they are not successful at preventing it.
- Lens preparation: Changes to the surface chemistry of the lens can also reduce the risk of PCO development. For example, UV/ozone treatment modifies the surface of the lens with no safety issues involved in the materials.
- Surgery type: Changes to the capsulotomy procedure may help to prevent secondary cataracts. Some researchers are investigating whether to leave the initial incision in the capsular bag open after implanting the IOL. This way, fluid in the eye can flow around the artificial lens, diluting and washing out remaining lens epithelial cells.
Working with a surgeon who doesn’t employ these techniques could increase your risks of complications, including secondary cataracts.
Key Facts About Secondary Cataracts
- About two in five people who have cataract surgery will develop a secondary cataract.
- Technological improvements, particularly in laser surgery, can help reduce PCOs. Researchers say incidence rates have declined to between 4 and 12 percent of patients due to advanced techniques.
- People who develop secondary cataracts often get them within 2 to 10 months after surgery.
- Procedures to fix secondary cataracts take about 5 minutes to complete. After surgical correction for secondary cataracts, most people can see better within about 24 hours.
Do Cataracts Come Back?
Your old cataract can’t come back, as the damaged tissues are removed during surgery.
Cataracts are cloudy areas in the lens of your eye, and surgery is the only cure. During that procedure, doctors remove the damaged lens and replace it with an intraocular lens (IOL). That synthetic lens can’t cloud or dim your vision.
But the IOL sits inside natural tissues, which can cloud and clump. When they do, a new cataract forms, and experts call this new one a PCO.

Cataract eye surgery is a very common and medically necessary procedure to remove and replace the eye’s natural lens when the vision has been clouded by a cataract. We offer laser-assisted cataract surgery and lifestyle lenses as options for our patients.
Learn More
How Are Secondary Cataracts Diagnosed?
After cataract surgery, your doctor examines your eyes regularly using specialized tools. If you develop a PCO, your doctor will see it during your exam.
When this condition is diagnosed, it will look like a wrinkled area on the back of the lens capsule, near the site of fusion of the top and bottom parts of the capsule.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
How Do Secondary Cataracts Develop?
The membrane around the lens capsule, which was not removed during cataract surgery and now contains the IOL, becomes cloudy and begins to impair vision. Proteins change, and new cells grow on the back of the capsule, obscuring your range of vision.
For PCO to develop, lens epithelial cells must do the following:
- Proliferate, or grow more of the problem cell
- Migrate, or move from one area to the problem area
- Differentiate from the residual lens epithelial cells (LECs) into a problem cell type
What Causes Secondary Cataracts?
Research published in 2017 investigated the molecular causes of secondary cataracts. Researchers uncovered a series of steps that can lead to PCOs.
Those steps include the following:
- Old cells from the lens, after it is broken up and removed from the capsule, remain on the epithelium of the capsule and begin to grow at the back.
- Growing cells may transform into two types of cells that can cause problems: lens fiber cells and myofibroblasts.
- The lens fiber cells will develop proteins called crystallins, causing light to scatter across the back of the eye as though it is being refracted through a crystal.
- Myofibroblasts create a matrix of molecules outside the cell, wrinkling the lens capsule so vision becomes obstructed.
The study investigated why epithelial cells from the old lens differentiate into these two problematic cell types. TGF-beta, a growth factor chemical, becomes active in response to surgery because the area must be healed. Typically, this is a wound-healing response, but an excess of activated TGF-beta in the area can influence these lens cells to migrate into other places before they begin to grow into different types of cells.
Some drugs that suppress TGF-beta are being tested to determine if they can prevent the formation of secondary cataracts, but the Food and Drug Administration (FDA) has not approved prescription drug treatments to prevent this condition yet.
What Are the Symptoms of Secondary Cataracts?
Secondary cataracts share many symptoms with other types of cataracts. Often, they cause noticeable vision issues.
Symptoms of PCO include the following:
- Blurry or dimmed vision
- Changes in your vision that aren’t relieved by new glasses prescriptions
- Inability to detect color changes or contrast
- Halos around lights
Some people also experience flares or flashes of light caused by LECs remaining in the capsule.
Can Problems Occur After a Secondary Cataract?
Although developing secondary cataracts is frustrating, treatment is relatively simple.
During a YAG laser capsulotomy, doctors use a laser to create a small opening in the clouded capsule so light can shine through to the retina. This surgery is painless and takes about five minutes.
There are some complications associated with this procedure, including these:
- Retinal detachment
- Damage to the IOL
- Partial dislocation of the IOL
- Cystoid macular edema
- Corneal edema
- Increasing intraocular pressure
- Hemorrhage in the iris
- Worsened localized endophthalmitis, inflammation in the interior of the eye
These risks are very low since the procedure does not take long, requires no incisions, and may not even require local anesthesia, depending on how your ophthalmologist will need to position the laser.
Some of these side effects are more likely to happen if you are very nearsighted or have a pre-existing eye condition like glaucoma.
If you develop any new symptoms — especially new “floaters,” seeing flashing lights, or a dark curtain moving up or down your vision — go back for a follow-up with your eye doctor immediately.
Secondary Cataracts Frequently Asked Questions
Do secondary cataracts get worse?
Without treatment, secondary cataracts can get worse. Cells within your eye can continue to grow and spread, further darkening your vision.
When should a secondary cataract be removed?
If you’re struggling to see clearly after cataract surgery, talk to your doctor. A quick medical procedure could fix the problem.
How do you fix secondary cataracts?
Doctors use a laser to create a small opening within the clouded capsule inside your eye. The procedure is painless and takes about 5 minutes to complete.
What is a secondary cataract called?
Secondary cataracts are sometimes called after-cataracts or posterior capsular opacification.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
References
- Researchers Focus on Preventing Secondary Cataract. (May 2016). Optometry Today.
- Types of Cataract. (January 2023). National Eye Institute.
- Findings Pave Way for Treatment of Secondary Cataracts. (April 2017). Optometry Today.
- Secondary Cataract: An Epidemiological and Clinical Survey at the Yaounde Gynaeco-Obstetric and Paediatric Hospital. (June 2011). Clinical Ophthalmology.
- What Is a Posterior Capsulotomy? (September 2022). American Academy of Ophthalmology.
- NIH-Funded Scientists Home in on Molecular Causes of Secondary Cataract. (March 2017). National Eye Institute.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.