
Medically Reviewed by Angelique J. Pillar, M.D.
Further Reading
Cataract Surgery Methods & Techniques (Compared)
Home / Guide to Cataract Surgery /
Last Updated:

Medically Reviewed by Angelique J. Pillar, M.D.
Although cataract removal surgery is considered an elective surgery it is a medically necessary surgery for millions of people all over the world. As technology improves, devices change or are added to the procedure that improve healing time, speed up surgery time, and boost overall outcomes for those who need cataracts removed.
For a long time, traditional cataract surgery was the only way to remove diseased lenses that had cataracts, replacing them with an artificial lens called an intraocular lens (IOL). However, as laser surgeries for eyes become more popular and the technology gets better, more eye surgeons are offering laser-assisted cataract surgeries. Few insurance companies cover this cost, but there are benefits to laser surgery.
Learn more here about both types of cataract surgery, so you can speak to your optometrist or ophthalmologist about which procedure might work best for you.
Table of Contents
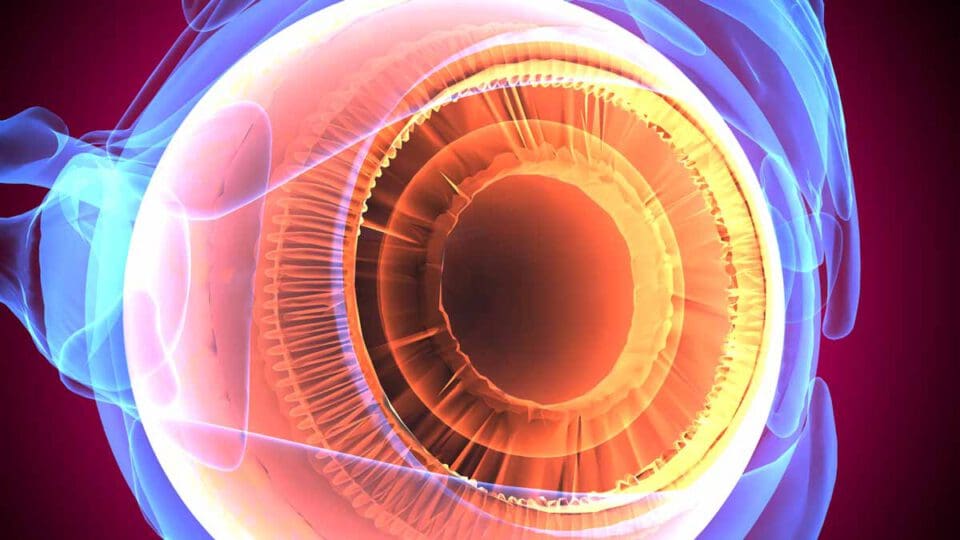
Why Do Cataracts Require Surgery?

Cataracts are a disease of the lens in the eye, which clouds vision, causes blurry or double vision, leads to yellowing of colors, and will eventually lead to blindness if untreated. If you get regular eye exams, it is likely that your optometrist will catch cataracts as they form at an early stage and can monitor how they develop. Eventually, your eye doctor may recommend cataract surgery to correct the issue once the problem becomes serious.
There are two basic types of cataract surgery — traditional or phacoemulsification surgery, and laser-assisted surgery — which lead to the same outcome: removing the diseased lens and replacing it with an artificial lens. The main difference between the two procedures is the tools used. Your eye surgeon will either use a scalpel or a laser to make very small incisions in your eye.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
There are some differences between the two procedures. Medical research is continuing to evaluate which operation has less impact and shorter healing times.
The Two Types of Cataract Surgery Methods
While the ultimate goal of cataract surgery is the same, there are two approaches to this surgery.
- Traditional cataract surgery: Also referred to as phacoemulsification, traditional cataract surgery involves a skilled surgeon making small incisions with a scalpel. First, the surgeon makes a very small incision in the cornea, so other instruments can make contact with the lens, which is behind the pupil. The surgeon then makes a circular incision in the lens capsule and inserts a pen-shaped probe that uses sound waves to break up the lens; the probe then suctions these pieces out of the eye. Once the diseased lens has been removed, the surgeon inserts an artificial lens called an intraocular lens (IOL). Typically, this is a monofocal lens of some type, although there are multifocal lenses that can be opted for at a higher price. Because the incisions are so small for most traditional cataract surgeries, the surgeon will likely insert a self-sealing liquid into the corneal incision, so you will not even have stitches.
- Laser-assisted cataract surgery: The steps involved in laser-assisted cataract surgery (LACS), including the more modern femtosecond-laser-assisted cataract surgery (FLACS), are the same as traditional cataract surgery. Your surgeon makes a small incision in the cornea and then the lens, breaks up the diseased lens, and replaces it with an IOL. Rather than use a scalpel, however, LACS procedures use lasers to create very small incisions in the eye. Lasers may also be used to break up the lens rather than sound waves. Laser-assisted incisions, like traditional cataract surgery incisions, will not likely require stitches and instead will involve self-sealing liquid.
If you have an astigmatism, your optometrist or ophthalmologist may recommend LACS because the procedure can be used to correct the astigmatism while also treating the cataract. If you opt for a premium intraocular lens like a multifocal lens, you may be offered LACS along with the upgraded lens. This is not because LACS and premium IOLs are both more expensive; rather, LACS allows your eye surgeon to position these lenses more precisely, so your eye can adjust to the new way of refracting light and seeing near and far objects more easily.
Thanks to medical research, we are learning more about the advantages and disadvantages between the two procedures, so in the near future, you may be able to choose between traditional and LACS for cataract surgery.
Advantages of Traditional Cataract Surgery
The benefits of traditional, or manual, cataract surgery are similar to LACS overall. Fast healing time will occur with a skilled surgeon just like it would with a programmed laser. There is a similar risk of complications like scars between the procedures.
The greatest advantage of traditional cataract surgery is the cost. A skilled surgeon will be covered by your insurance because cataract removal is considered medically necessary. However, most insurance companies will not cover laser-assisted procedures because the expense of the machine is not currently considered medically necessary, as it does not dramatically improve healing or impact in this outpatient procedure. Some medical research does show that there may be some healing improvements with LACS.
Some studies have found that there are slightly fewer complications associated with traditional cataract surgery compared to LACS. Posterior capsule complications were reported in 0.7 percent of eyes treated with FLACS compared to 0.4 percent of eyes treated with manual surgery. Other post-operative complications were seen in 3.4 percent of FLACS compared to 2.3 percent for manual.
Although refractive errors like nearsightedness were more improved with FLACS overall, studies show that people who underwent manual cataract surgery could read more letters at a distance compared to those who underwent FLACS. There were higher general rates of errors in FLACS compared to manual surgery, although this will change as more surgeons train in FLACS.
A 2016 study found that rates of posterior capsule opacification (PCO) in the first three months after cataract surgery were higher among patients who had undergone FLACS compared to manual surgery. Among the 29 FLACS patients, 7 cases reported PCO at three months and required a capsulotomy; out of 50 manual cataract surgery patients, none needed this procedure.
The Disadvantages of Traditional Cataract Surgery
If you need surgery to remove your cataracts, there are few disadvantages to traditional surgery, especially compared to FLACS. One major disadvantage involves different IOLs. If you choose a premium IOL, you will receive greater benefit for the overall fit and vision adjustment period if you pursue LACS, which has the preprogrammed precision to insert multifocal or toric lenses. While many eye surgeons can perform this procedure manually with consistent success and few complications, there is less risk with FLACS for these lenses.
As FLACS surgeries improve, there are greater overall vision improvements, especially with refractive errors like nearsightedness, farsightedness, and astigmatism, compared to manual surgery. People who have long struggled with a refractive error, and later developed cataracts, may wish to pursue LACS rather than manual surgery.
Someday, the advantages of laser-assisted cataract surgery may outweigh those of traditional cataract surgery, but most eye surgeons agree that currently both procedures are largely effective in improving vision.
Advantages of Laser-Assisted Cataract Surgery, Including New Types of Laser Surgery
Studies of femtosecond-laser-assisted cataract surgery (FLACS) find that the improved precision from lasers allows for very specific incisions in the cornea and lens capsule. If needed, these incisions are so precise that they can be repeated in follow-up surgeries. This procedure also reduces the amount of energy required for the ultrasound device to break up the lens for removal.
There are two main incisions in cataract surgery: the arcuate or corneal incision, and the capsulorhexis or lens capsule incision. Surgeons report that 90 percent depth into the cornea is the optimal incision depth, and using machine-calibrated lasers to make this incision allows for even greater precision. The capsulorhexis incision must be circular, and a programmed machine can use its laser to make a perfectly circular incision, which human hands — as skilled as they may be — cannot do.
Lasers can be adjusted so there is a smaller external width than the incisions produced by a scalpel, so there is less wound leakage. These machines also allow for much greater range of motion on the surgeon’s part, which is important with an organ as small and delicate as the eye.
With the help of a laser to soften the lens itself, the amount of ultrasound energy used to break up the cornea is reduced, which decreases the amount of trauma to the eye. One study reported that the laser softening was helpful when the cataracts were hard.
Because of the precision, there are few complications associated with the procedure, and most patients can tolerate FLACS well. The rate of visual recovery, including from refractive errors like astigmatism, is promising. Among people treated with FLACS, 89.7 percent reported greater than 20/30 vision compared to 84.2 percent who were treated with manual surgery. More people reported better than 20/40 vision with FLACS versus manual: 96.6 percent compared to 93.9 percent, respectively.
A retrospective survey examined 3,784 cases of manual cataract surgery and 3,371 instances of FLACS surgery between 2010 and 2012. The data showed that rates of vitreous loss were lower overall in the FLACS group, which can change how well the eye heals.
Disadvantages Associated with Laser-Assisted Cataract Surgery
There are a few disadvantages to LACS.
- It is expensive. This is true both for the patient, because insurance may not cover all of the procedure, and for the surgeon. The equipment and training required to perform LACS mean a significant upfront investment after the surgeon has already trained in traditional cataract surgery. There are also constant improvements being made to laser technology, making it faster, more precise, and less reliant on specific room temperatures or other conditions. This means an eye surgery center will likely require ongoing investment in their technology.
- There is increased surgery time. In many cases, the laser that makes the incisions must be set up in a separate room from other equipment, like the ultrasound probe, so the patient must be transferred from one room to another, increasing the time of the overall procedure.
If you do not have a specific reason to pursue laser surgery, either as a patient or as an eye surgeon, it may be best to opt for manual surgery for now.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
Which Cataract Surgery is Best?
Phacoemulsification (phaco) and extracapsular extraction are the two primary types of cataract surgery. Both are relatively safe outpatient procedures and involve the removal of affected (clouded) eye lenses under local anesthesia.
After the cloudy cataract is extracted, an artificial implant called intraocular lens (IOL) may be inserted in its place. You may be prescribed external contact lenses if an implant isn’t right for you.
Both procedures are also similar in their approach if you need to correct cataracts in both eyes. Doctors will operate on one eye at a time. The span between two eyes can be as little as a few days to several weeks or months depending on the individual lens in each eye and the recovery from the first procedure.
Phacoemulsification
During phaco cataract surgery, your ophthalmologist creates a tiny opening around the edge of the cornea. A small instrument that produces ultrasounds is inserted in the incision.
The transmitted waves break up the lens into fragments. Your surgeon uses a suction device to draw the tiny debris out of the cornea.
Almost in all cases, an intraocular lens will be placed in the eye. This lens stays in the eye permanently to restore your eyesight.
With phaco, the incision rarely needs sewing after IOL insertion because it’s usually small enough to close and heal naturally.
Today, most ophthalmologists in the developed world perform phaco cataract surgery, and it is considered to have several advantages.
These include:
- Slightly better visual outcomes
- The small surgical incision on the cornea allows for faster recovery
- You’re unlikely to experience astigmatism (blurred near or far sightedness) because no stitching is required after surgery
While your doctor will explain these considerations to you, keep in mind that phaco surgery is generally the most expensive option.
Extracapsular Cataract Extraction (ECCE)
Unlike phaco, extracapsular cataract extraction (ECCE) doesn’t require breaking up the lens with cataract. Instead of using an ultrasound device for this purpose, your ophthalmologist will manually cut the entire lens out, in one piece.
An extended cut around the edge of the cornea is usually necessary to extract the cataract this way. Next, an IOL can be placed in the empty lens capsule.
The larger surgical incision will be sewn shut.
While ECCE is generally cheaper than phaco, it isn’t offered to patients with routine cataracts because of the longer recovery time and larger incisions. Many ophthalmology programs no longer teach the ECCE technique as most cataracts are able to be removed with modern phaco. Even so, some doctors would recommend ECCE for the removal of certain advanced cataracts.
These include when:
- The cataract is too dense to dismantle using ultrasound waves
- The back of the affected lens raptures during phaco surgery (tearing of the posterior capsule)
Potential post-surgery issues among ECCE patients are:
- Slower recovery time
- There’s a higher likelihood of developing astigmatism due to the stitching
Intraocular Lens (IOL) Options
Eye tests before surgery will determine the best IOL implant to restore your eye’s focusing power. Based on your personal preferences and budget, you can select specific features for your artificial lens replacement.
Common types of IOL implants include:
- Monofocal lenses
- Multifocal lenses
- Extended depth-of-focus implants
- Accommodating Implants
- IOL Implants
Monofocal Lenses
A monofocal lens corrects either nearsightedness or farsightedness at a time, but not both. If you chose this type of artificial implant, you can have it designed to only fix distance vision.
You may then get reading glasses to correct near vision. Alternatively, get a near-vision IOL for one eye and a distance-vision IOL for the other.
Multifocal IOLs
Multifocal lens implants can correct both nearsightedness and farsightedness simultaneously. Getting these premium lenses minimizes the need to use reading glasses. Some of these optical devices may have extra corrective areas for intermediate focusing.
Extended Depth-of-Focus (EDOF) Implants
Extended depth-of-focus implants (EDOF) can adjust to let you see far or near objects more clearly. Unlike multifocals, they don’t feature multiple corrective zones.
Accommodative IOLs
When you get accommodative plastic lenses, you get near, intermediate, and distance vision improvements. Their point of focus shifts along with your natural eye muscle movements.
Toric IOL Implants
Toric IOLs can correct astigmatism. They’re generally a good option for patients who may develop this eye defect after getting corneal sutures.
Light Adjustable IOLs
Adjustable intraocular lenses are a premium lens that allows for your doctor to change the power of your lens and correct your astigmatism after the cataract surgery is already done. These lenses are made of silicone that reacts to light and allows your doctor to change the power of your lens. This lens is good for patients with prior refractive surgery or those that desire a customized outcome.
Removing Cataracts Improves Quality of Life

The American Academy of Ophthalmology (AAO) notes that both traditional and laser-assisted cataract surgeries have similar recovery times. One is not inherently better than the other for recovery. There are also similar rates of complications and errors between the surgeries, so the biggest difference is in out-of-pocket cost.
Traditional cataract surgery is considered a medically necessary procedure when it is recommended, so most insurance companies will cover the cost. However, LACS is more controversial on this front. Rarely is LACS covered by the insurance company and is considered a self-pay add-on.
Once you have cataracts removed, you will notice immediate improvements in your overall vision; however, you may not get the vision you had when you were much younger. There are several age-related or trauma-related eye conditions that can affect your vision along with cataracts. This may mean that you still require glasses or contact lenses after your cataract surgery, but you will no longer experience the fuzziness, vision loss, double vision, or color changes in your vision that are caused by cataracts.

Cataract Surgery
Cataract eye surgery is a very common and medically necessary procedure to remove and replace the eye’s natural lens when the vision has been clouded by a cataract. We offer laser-assisted cataract surgery and lifestyle lenses as options for our patients.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
References
- What Are Cataracts? American Academy of Ophthalmology (AAO).
- Traditional Cataract Surgery vs. Laser-Assisted Cataract Surgery. (August 10, 2017). American Academy of Ophthalmology (AAO).
- A Review of Laser-Assisted Versus Traditional Phacoemulsification Cataract Surgery. (June 2017). Ophthalmology and Therapy.
- The Pros and Cons of Femtosecond Laser-Assisted Cataract Surgery. (September 3, 2015). EyeOpener.
- The Advantages of Femtosecond Laser-Assisted Cataract Surgery. (January – March 2015). Romanian Journal of Ophthalmology.
- Cataract Surgery. WillsEye Hospital.
- Outcome of Phacoemulsification and Extracapsular Cataract Extraction: A Study in a District Hospital in Malaysia. (August 2014). Malaysian Family Physician.
- Manual Cataract Extraction Taught Less but Still Needed. (January 2013). American Academy of Ophthalmology.
- Choosing an Artificial Lens for Cataract Surgery. (May 2014). American Academy of Ophthalmology 2021.

Angelique J. Pillar, MD is a fellowship trained and board certified ophthalmologist specializing in cataract, cornea, and refractive surgery.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.