Further Reading
Pigmentary Glaucoma: Prognosis, Timelines & Treatment
Home / Diagnosed With Glaucoma /
Last Updated:

Article At a Glance
Pigmentary glaucoma is a rare form of glaucoma that typically affects younger, nearsighted adults. It happens when pigment from the iris flakes off and clogs the eye’s drainage system, increasing eye pressure and risking vision loss. With early detection and consistent care, vision can often be preserved. If you’re at risk or experiencing symptoms, talk to your eye doctor about getting checked.
Table of Contents
Pigmentary glaucoma goes hand in hand with pigment dispersion syndrome. People with this condition flake pigment from their eyes, and sometimes, that pigment accumulates and blocks drainage ducts. When that happens, glaucoma sets in.
There are two types of glaucoma: open-angle glaucoma and angle-closure glaucoma (also called narrow-angle glaucoma). Pigmentary glaucoma is an open-angle form of the condition.
Pigmentary glaucoma is most common in young, nearsighted males. Symptoms are subtle, and they include haloes around lights.
Treatment aims to reduce pressure, not keep pigment in place. Eye drops and surgeries are often used to help preserve sight. The condition tends to fade with age, but lost eyesight can’t be restored. Treatment is critical.
Researchers are hard at work to find new therapies for pigmentary glaucoma. Recently, studies uncovered a genetic link to the condition. That could result in treatment innovations in time.
What Is Pigmentary Glaucoma?

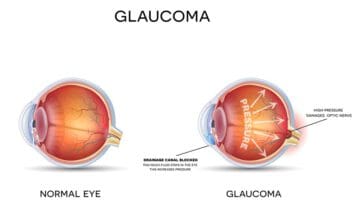
There are multiple forms of glaucoma, and all involve pressure. When your eye can’t process fluids properly and they build up within the eye, the optic nerve can be damaged. That can result in vision loss.
Glaucoma can stem from many triggers. Pigmentary glaucoma originates in the colored part of your eye, known as the iris.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
Whether your eyes are blue, green, or brown, they owe that color to pigment granules within the eye. Those bits of shade should stay in place no matter what you do. But in some people, those pigment bits break away and collect within the eye. Sometimes, they are harmless debris, but they can band together and do damage.
In some people, those pigment bits clump together. The eye attempts to flush out the blockage through drainage channels. But if the pigment block is big enough, the eye can stop draining altogether.
Your eye continues to create fluid, even if none is moving out. Pressure begins to rise as fluid builds up with nowhere to go. That pressure can squeeze the optic nerve, and sometimes, it damages that critical pathway. Vision loss results.
If pigment blocks fluid processing, pigmentary glaucoma is an appropriate diagnosis.
Terminology Recap: Open-Angle Glaucoma & Angle-Closure Glaucoma
As we mentioned, many forms of glaucoma exist. They can be split into two groups based on how the disease progresses.
The Glaucoma Research Foundation explains that there are two main glaucoma types.
- Open-angle glaucoma: Drainage canals leading out of the eye close slowly, and pressure begins to rise. The issue starts small, and it’s very easy to ignore. Without treatment, permanent vision loss can result.
- Angle-closure glaucoma: This is a less common form of glaucoma, and it’s characterized by a sudden block of the drainage canals. Symptoms are noticeable right away.
The University of Arizona says that pigmentary glaucoma is an open-angle form of the disease. That means symptoms start small, and in some cases, they could be ignored altogether.
Which Form of Glaucoma Is Pigmentary Glaucoma?
Pigmentary glaucoma is a type of open-angle glaucoma, a vision problem that has no noticeable warning signs. It is the most common glaucoma, and it occurs with a wider and open angle between your iris and the cornea.
When you have this chronic condition, pigment dispersion takes place gradually as does the accumulation of the dispersed debris in your eyes. Blockage of the fluid drainage canals in the eyes continues as pressure builds up.
If you have pigmentary glaucoma, you won’t experience any significant symptoms, including vision damage, for the most of your life. But you could lose your eyesight if you don’t have regular eye checkups, which would discover any abnormal eye pressure before irreversible damage can occur.
Fortunately, changes in eye pressure because of pigment dispersion syndrome (PDS) are detectable, including the onset of glaucoma. If a doctor discovers this condition during one of your eye exams, you can undergo early treatments, a major deterrent against developing pigmentary glaucoma.
Risk Factors for Pigmentary Glaucoma
The pigment within your eyes should stay put. But for some people, eye structures are irregular, and that allows color to flake away.
Your iris should be curved outward, as is the shape of your eye. In some people, the iris is flat or concave. Each time you squint, blink, or move your eye, the unusual iris rubs on other parts of the eye. In time, bits of the iris can flake away under the pressure. This is known as pigment dispersion syndrome.
The BrightFocus Foundation says you could be at risk for pigment dispersion syndrome if you:
- Are male.
- Have nearsightedness (myopia).
- Are between 20 and 40 years old.
- Have a family history of the disorder.
Your eye doctor can spot the condition during a standard eye exam. Spots of color may appear in unusual places. When doctors use a slit lamp to check your iris, they’ll see spots that have no pigment at all.
You can have pigment dispersion syndrome without glaucoma. In fact, the BrightFocus Foundation says just 30 to 35 percent of people with the syndrome develop glaucoma.
Symptoms of glaucoma are subtle. In the beginning, you may notice:
- Blurry vision.
- Haloes around lights.
- Headaches.
- Nausea or vomiting.
These symptoms may worsen when you are engaged in impact sports like basketball or soccer.
In time, these symptoms can worsen. You may then notice difficulty with your vision, including gaps in your visual field.
There is no specific pigmentary glaucoma timeline. Your disease will progress at a clip dictated by your pigment loss. Some people develop serious problems within months, and in others, it can take years.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
Does Exercise Cause Pigmentary Glaucoma?
There’s no doubt that intense physical activity like jogging, kick boxing or playing basketball can trigger pigment dispersion. The connection between PDS and glaucoma is well established, too.
These correlations raise concerns over the safety of exercise when you have PDS. However, each patient is different, and there’s no guideline for or against exercising when you have this condition.
Once you’re diagnosed with PDS, you should ask your eye doctor if you can work out without increasing you risk of developing pigmentary glaucoma. You’ll probably need continuing monitoring and periodic eye pressure tests after your PDS diagnosis.
If vigorous exercise causes you to experience alarming increases in eye pressure, your doctor may advise against it. However, many PDS patients can jog or cycle without any appreciable changes in eye pressure.
One study involving patients with PDS indicated that workouts caused only a negligible increase in pigment disintegration and eye pressure. The patients’ pressures returned to normal within 30 minutes after exercise.
Treatment Options for Pigmentary Glaucoma

The goal of therapy is not to keep pigment where it belongs. Instead, professionals use treatments to lower the pressure in your eye.
The Glaucoma Research Foundation says it’s very difficult to stop pigment loss in the eye. But doctors have many methods they can use to reduce eye pressure.
Your doctor might use:
- Eye drops. These medications reduce eye pressure, and you can use them at home.
- Pupil constrictors. These medications keep your eye closed tight so structures will not rub together.
- Laser surgery. Your doctor uses precise tools to help the eye drain effectively so pigment will not build up. Your doctor can also use lasers to amend the shape of the iris so it will not rub on surrounding structures.
It’s critical to get care for pigmentary glaucoma, as the vision loss you experience will not ever come back. But time could help to improve the disease.
The American Academy of Ophthalmology explains that pigment loss may stop as people get older. Aging eyes don’t move as much as their younger counterparts, so less friction occurs. Your eyes may also change shape as you age, so the iris is farther from irritating neighbors.
Future Treatment Options
It might be discouraging to hear that there is no cure (aside from age) for pigmentary glaucoma. But researchers are hard at work on solutions, and recent discoveries hold a great deal of promise.
In 2019, researchers discovered a gene that could be responsible for pigmentary glaucoma. They hope that this discovery could help them to develop therapies that could halt the disease in vulnerable people, long before it begins. Gene identification could also help people pinpoint risks, so they can take preventive steps to reduce eye pressure before vision loss sets in.
These therapies will not be sitting in your doctor’s office in the near future. Researchers need time to develop therapies and test them. But this exciting discovery could help future generations to preserve their sight, even when they are living with a serious condition.
In the interim, if you’ve been diagnosed with pigmentary glaucoma, work with your doctor and follow your treatment plan carefully. That is the best way to ensure that you do not experience permanent vision loss.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
References
- Types of Glaucoma. (October 2017). Glaucoma Research Foundation.
- Glaucoma, Pigment Dispersion Syndrome. The University of Arizona Health Sciences.
- Pigment Dispersion Syndrome and Pigmentary Glaucoma. (October 2019). Glaucoma Research Foundation.
- Pigmentary Glaucoma and Pigment Dispersion Syndrome. (September 2015). BrightFocus Foundation.
- Pigmentary Glaucoma: 24-Year-Old Male with Episodic Haloes Around Lights and Blurry Vision. (February 2014). University of Iowa Health Care.
- Pigmentary Glaucoma: Answers to Your Questions. (April 2018). Glaucoma Research Foundation.
- Pearls for Care in Pigmentary Glaucoma. (May 2015). EyeWorld.
- Pigmentary Glaucoma. American Academy of Ophthalmology.
- Scientists First to Pinpoint a Cause of Pigmentary Glaucoma. (January 2019). Medical Xpress.
- Ocular Urban Legends. (November 2014). Review of Optometry.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.