Guide to Macular Pucker: What Is It & Is Surgery Always Needed?
Home / Eye Conditions & Eye Diseases /
Last Updated:
Table of Contents
Your macula is part of your retina, located at the back of your eyeball where the visual process begins. A macular pucker occurs as part of the aging process, and it is the result of scar tissue on the macula.
The major risk factor for the development of a macular pucker is getting older, but there are some additional factors in play.
A macular pucker is different from a macular hole, and it is not the same thing as macular degeneration.
The damage associated with a macular pucker is typically not progressive. For most people, the symptoms are mild.
An optometrist will usually diagnose a macular pucker. In most cases, treatment will not be needed, or the use of corrective lenses will be sufficient.
If the symptoms of a macular pucker are severe, surgery may be recommended. On average, surgery restores 50 percent of lost eyesight, but the results can be variable.
What Is the Macula?
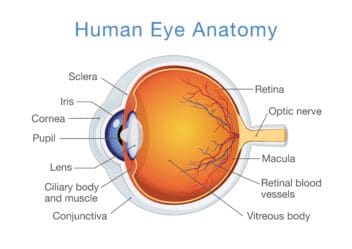
The sense of vision requires physical energy from the environment to be translated in your brain to visual images. The area where this begins is the retina, the sensory membrane that lines the inner surface of the back of your eye. It has several layers.
In the center of the retina is an area called the macula. At the center of the macula, there is a small depression, the fovea, where photoreceptor cones are concentrated. This area is responsible for maximal visual acuity and color vision.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
What Is a Macular Pucker?
A macular pucker refers to scar tissue that has developed in the macula. Scarring of the macula can lead to distorted vison or even blurry central vision, damaging the ability to see fine details in the center of your visual field.
The terms retina wrinkle, premacular fibrosis, and surface wrinkling retinopathy all refer to a macular pucker.
What Causes a Macular Pucker?
Most of your eye is filled with a thick gel-like substance that is known as vitreous humor or just referred to as the vitreous. It fills about fourth-fifths of your inner eye.
The vitreous humor contains millions of fibers that are connected to the retinal surface. As people get older, the vitreous humor slowly shrinks and moves away from the surface of the retina, leading to what is often referred to as a vitreous detachment.
This is a normal aspect of aging, and in most cases, it is relatively benign. In some cases, there can be damage to the retinal surface during this process.
The damaged area will heal and may leave a scar on the surface of the retina. When the scar tissue contracts, it leaves a wrinkle on the retina, which is often referred to as a pucker.
If the scar tissue is formed over the macula as this process occurs, you can develop a macular pucker. This macular pucker can affect your central vision.
Risk Factors for the Development of a Macular Pucker
Getting older is the major risk factor for the development of a macular pucker, as the process that forms a macular pucker is usually age-related. Some other risk factors include:
- Swelling inside the eye.
- Previous eye surgery or serious eye damage from an eye injury.
- Problems with the vasculature in the retina that impairs blood flow.
- A torn or detached retina.
Different Than a Macular Hole
A macular pucker is simply a wrinkle that occurs as a result of the above process, whereas a macular hole might occur when the process results in the virtuous humor actually separating part of the macula from the retina.
Of course, holes in the retina and macula can occur from other processes as well.
Not the Same as Macular Degeneration
Although the symptoms can be similar, a macular pucker is a different condition from macular degeneration (also referred to as age-related macular degeneration).
Macular degeneration involves the breakdown of the macula, whereas a macular pucker occurs according to the process described above. Macular degeneration is a progressive disease and the most common cause of visual loss in people over the age of 60.
Not Progressive
Macular Pucker Progression
Macular pucker does not get progressively worse over time for most people. Visual acuity usually remains stable.
A retrospective observational study conducted between 2012 and 2015 to predict the progression of untreated macular pucker using optical coherence tomography (OCT). Results showed that visual acuity of 80 percent of the patients stayed the same or improved during the observation period.
Researchers wanted to evaluate changes in visual acuity and central subfield thickness, issues that sometimes affect people with macular pucker, between initial doctor visits and follow-up appointments. But for 468 patients who had untreated macular pucker, visual acuity and central subfield thickness did not change during an observation period of 448 days.
Although macular pucker usually strikes only one eye, it’s possible the other eye could be affected. However, that secondary condition is not prevalent.
You deserve clear vision. We can help.
With 135+ locations and over 2.5 million procedures performed, our board-certified eye surgeons deliver results you can trust. Your journey to better vision starts here.
Symptoms of a Macular Pucker

The symptoms can be variable and range from no visual problems at all to severe visual loss, although severe visual loss is rare.
Common symptoms include blurry vision, distorted vision, and straight lines appearing to be wavy. A gray area or blind spot in the center of vision may be present. Often, there will be difficulty distinguishing fine detail, such as reading small print.
Diagnosis of a Macular Pucker
Diagnosis is most often made by an ophthalmologist during a routine eye examination.
The ophthalmologist will dilate your pupils in order to view the inside of your eye and may take pictures using optical coherence tomography (OCT). By studying the pictures, the ophthalmologist can determine the source of the problem.
Treatment
You may not need any treatment for mild symptoms of macular pucker, including blurriness and vision distortion. Your eye doctor can recommend bifocals or an updated eyeglass prescription to improve your vision.
Most people often adjust to the minor visual distortion caused by macular pucker because it rarely affects daily activities such as driving or reading. Medications, eye drops and nutritional supplements are not effective against macular pucker.
In some cases, macular pucker clears up when the causative scar tissue detaches from the retina. Surgery becomes the only viable option when your vision worsens to the point where it affects your routine daily activities. Surgery to repair a macular pucker involves a procedure known as vitrectomy, and it is considered rare.
How Does Surgery for a Macular Pucker Work?
Vitrectomy is a surgical procedure to remove some or all of the vitreous humor from your eye. This procedure is done to prevent the vitreous humor from pulling on the retina. The eye surgeon replaces the vitreous humor with a salt solution. Vitreous humor is mostly water. As such, patients will not notice any changes between the two fluids. Following vitrectomy, doctors perform an additional procedure known as membranectomy. Membranectomy is the removal of tissue layers from the retina using minute instruments. This layer of unhealthy tissue is known as the epiretinal membrane and can form scar tissue characteristic of macular pucker. Note that there are some complications that vitrectomy surgery can bring about. The most frequent complication is the development of cataracts within a few years after the surgery. This often requires further surgery to remove cataracts. Other potential complications may include:
- Eye infections
- Bleeding in the eye
- Separation of the retina from the back of the eye (retinal detachment, a rare occurrence)
- Retinal edema
- High intraocular pressure
Does the Surgery Work?
On average, about 50 percent of vision that is lost as a result of a macular pucker is restored by the surgical procedure, but results will vary. In most cases, full vision is not restored.
Recovery can take up to three months.
Recovery from Macular Pucker Surgery
Following surgery, you will use eye drops for several weeks to enable the surface of your eye to heal and to prevent infections. It may be necessary to wear an eye patch temporarily to protect your eye for a few days or weeks. And it may take up to three months to fully recover from macular pucker surgery.
Sometimes, the eye surgeon may place a gas bubble inside your eye to keep your retina in place. If this is the case, you will need to maintain certain head positions. The bubble dissolves over time.
Prevention of Macular Pucker
There are no definitive prevention measures for macular pucker. However, your eye doctor can screen for macular pucker and other macular conditions with routine eye exams.
As such, visiting your eye specialist regularly is recommended especially if you are a candidate for the aforementioned risk factors. In between your eye exam appointments, you can also self-monitor using the Amsler grid.
References
The Retina. (May 2017). MedlinePlus.
The Function of a Normal Macula. (July 2015). BrightFocus Foundation.
Macular Pucker. (April 2019). The Cleveland Clinic.
What Is the Virtuous Humor? (May 2017). WebMD.
Macular Pucker Causes. (August 2019). American Academy of Ophthalmology.
Facts About Macular Hole. (April 2012). National Eye Institute.
Facts About Age-Related Macular Degeneration. (November 2018). National Eye Institute.
What Conditions can OCT Help to Diagnose? (June 2019). American Academy of Ophthalmology.
Vitrectomy. (2016). American Society of Retina Specialists.
Predicting Progression of Macular Pucker. (August 2020). Ophthalmologica Journal.
Macular Pucker. (July 2019). National Eye Institute.
What is retinal pucker surgery? Macula Center.
Surgery for post-vitrectomy cataract. (July 2008). Cochrane Database of Systematic Reviews.
Vitrectomy surgery of diabetic retinopathy complications. (2016). Romanian Journal of Ophthalmology.
Macular Pucker. (The Eye Institute for Medicine & Surgery).
Macular Pucker Prevention (December 2019). NYC Retina.
This content is for informational purposes only. It may have been reviewed by a licensed physician, but is not intended to serve as a substitute for professional medical advice. Always consult your healthcare provider with any health concerns. For more, read our Privacy Policy and Editorial Policy.